 |
 |
AbstractPurposeThe shortage of pediatric emergency care has become a significant societal issue. This study investigated the usage pattern of emergency departments (EDs) by pediatric patients who underwent interfacility transfers (IFTs) in South Korea, focusing on cases involving single and double IFTs.
MethodsThis nationwide cross-sectional study included all pediatric patients (< 19 years) who underwent IFTs at regional and local emergency medical centers from 2016 through 2018, using data from the National Emergency Department Information System. After excluding unidentified cases, clinical features and ED use patterns were compared between patients with single IFT, i.e., an IFT after the initial ED visit, and those with double IFT, i.e., a sequential transfer from one medical facility to another.
ResultsAmong 20,888 pediatric cases of IFTs in the ED, 21.0% of disease cases (3,070/14,624) and 11.4% of injury cases (691/6,038) experienced double IFTs. The double-transfer group showed a lower proportion of high acuity than the single-transfer group (22.6% vs. 15.0%; P < 0.001). However, median values of ED length of stay were longer in the double-transfer group, regardless of type of cases (disease: 163 minutes [single] vs. 218 minutes [double]; injury, 111 minutes vs. 172 minutes; all Ps < 0.001). GuardianвҖҷs request was a substantial reason for double IFT (disease, 29.9% [919/3,070]; injury, 56.4% [390/691]).
ConclusionDouble IFT is common in pediatric patients and strains medical resources, regardless of severity. The high occurrence of double IFT driven by guardiansвҖҷ requests rather than medical emergencies underscores the need for improved awareness of the emergency medical system among pediatric patientsвҖҷ caregivers.
IntroductionPediatric emergency departments (EDs) are critical units of healthcare systems designed to meet childrenвҖҷs unique needs and vulnerabilities (1). Because of the distinct characteristics of pediatric patients, many physicians limit their clinical practices to adults (2). While the shortage of specialized pediatric emergency resources has become increasingly apparent (3,4), the number of interfacility transfers (IFTs) of pediatric patients has increased over time (5). According to data from 42 tertiary care pediatric hospitals in the United States, two-fifths of the IFTs of pediatric patients were classified as potentially avoidable cases, of which half received no medical or procedural intervention upon arrival at the receiving hospitals (6).
IFT is defined as a transfer, after initial assessment and stabilization, from and to a health care facility, including hospital to hospital, clinic to hospital, hospital to rehabilitation, and hospital to long-term care (7). IFT inherently poses risks, including delays in care, miscommunication between referring and receiving hospitals, the omission of crucial medical information, and the occurrence of adverse events during transport (8,9). Many studies have reported that patients undergoing IFTs showed worse outcomes and increased financial costs (9-11). Additionally, the incidence of adverse events during IFTs of pediatric patients ranged from 10% to 20% (12,13). Considering the complexity and vulnerability of such patients and potential risks of IFTs, they should be carefully determined (14).
Therefore, it is essential to note innovative strategies that reduce the prevalence of potentially avoidable IFTs and enhance the emergency care system. Understanding the characteristics of patients undergoing IFT is pivotal to developing effective strategies, particularly in cases of double transfer, i.e., sequential transfer from one medical facility to another. In this study, we aimed to investigate the patterns of ED utilization among pediatric patients undergoing IFTs in South Korea, focusing on cases involving single and double IFTs.
Methods1. Study design and populationThis nationwide cross-sectional study used data from the National Emergency Department Information System (NEDIS), which is a data registry that includes more than 98% of all EDs in South Korea. The data are managed and qualified by the National Emergency Medical Center, a government-funded national ED control organization. From 401 EDs in South Korea, we compiled the data of 36 regional and 117 local emergency medical centers (EMCs), of which clinical data are highly reliable. The regional and local EMCs are equivalent to level I and II centers in the U.S., respectively. The National Emergency Medical Center approved the use of the anonymized NEDIS dataset, and ethical approval for this study was waived by the institutional review board because it used a publicly available anonymized dataset (IRB no. 2020-1818).
This study included pediatric patients under 19 years of age who underwent IFTs at the abovementioned EMCs from 2016 through 2018. We excluded cases of missing critical information. The included cases were categorized into single- and double-transfer groups. Patients with single IFT were defined as those who visited the ED from the scene without going through a healthcare facility and were transferred to another healthcare facility after the ED examination. Patients with double IFT, defined as those who were transferred from other healthcare facilities to the ED, underwent sequential transfers from the initial ED to another. We compared the clinical features and ED use patterns of patients with single and double IFTs.
2. Data collectionThe demographic and clinical data of the patients, including age, sex, mode of ED arrival, causes of ED visits (disease or injury), Korean Triage and Acuity Scale (KTAS) level, primary diagnosis code at ED discharge, ED length of stay (EDLOS), severe diagnosis, and reason for IFT, were extracted from the NEDIS database (15). Their cases were categorized into 4 age groups (< 1, 1-5, 6-11, and 12-18 years). They were also categorized into 3 groups according to a KTAS level: high (levels 1-2), moderate (level 3), and low acuity (levels 4-5). The primary ED diagnoses used the Korean Classification of Diseases, seventh Revision. Codes of the severe diagnoses consist of 28 code groups, such as cerebral infarction, gastrointestinal bleeding or foreign bodies, acute myocardial infarction, intracranial hemorrhage, and major trauma, as designated by Korean government (16).
3. Statistical analysisWe conducted a case-based analysis, as a single patient could have visited an ED multiple times. Continuous variables were represented as medians (interquartile ranges) according to their nonnormal distribution in the Kolmogorov-Smirnov test. Categorical variables were expressed as absolute numbers (percentages). The demographic and clinical characteristics between the single- and double-transfer groups were compared using the Mann-Whitney U-tests and chi-square tests for continuous and categorical variables, respectively. Two-sided P values < 0.05 were considered statistically significant. All statistical analyses were performed using IBM SPSS ver. 21.0 (IBM Corp.).
ResultsIn total, 4,386,311 pediatric cases from the regional and local EMCs were reported during the study period, with 20,888 (0.5%) requiring IFTs from the EDs to other medical facilities (Fig. 1). Among the 14,624 disease cases, 3,070 (21.0%) underwent double IFTs. In the 6,038 injury cases, 691 (11.4%) underwent double IFTs.
Table 1 demonstrates the baseline features of cases of the single- and double-transfer groups. Double IFTs were more frequent in the most age groups, except 1-5 years. The percentage of cases that arrived at the EDs via public emergency medical services was lower in the double-transfer group than in the single-transfer group (32.6% vs. 3.1%). The proportion of high-acuity cases was lower in the double-transfer group. Double IFTs occurred more frequently in the regional EDs (31.4% vs. 45.4%) than in the local EDs. In disease cases, the double-transfer groups had a higher rate of severe diagnosis (15.1% vs. 17.7%), whereas in injury cases, the equivalent rate was higher in the single-transfer group (20.2% vs. 16.1%).
Median values of EDLOS were longer in the double-transfer group, regardless of type of cases (disease, 163 minutes [single] vs. 218 minutes [double]; injury, 111 minutes vs. 172 minutes) (Table 2). The proportions of EDLOS longer than 6 hours were higher in the double-transfer group than in the single-transfer group.
Regarding the referred hospitals, specialty acute care hospitals were most common in both groups of disease cases and the single-transfer group of injury cases. In contrast, community hospitals were most common in the double-transfer group of injury cases. Among the reasons for transfer-out, the unavailability of medical resources was most common in disease cases, while a guardianвҖҷs request was most common in injury cases.
DiscussionIn this nationwide cross-sectional study, we observed that 21.0% of transferred pediatric disease cases and 11.4% of injury cases underwent double IFTs from one ED to another, indicating a prevalence of the phenomenon. Our study findings on the ED use pattern related to double IFTs demonstrate that double IFTs consume more ED resources than single IFTs. Moreover, this resource-consuming process was largely driven by the guardiansвҖҷrequests, particularly in injury cases, rather than medical needs, suggesting the need to improve societal perceptions regarding pediatric emergency care systems.
The overall proportion of IFT cases at the EDs was relatively low at 0.5% among all pediatric patients visiting the regional or local EMCs. However, it is worth noting that 11.4% (injury) to 21.0% (disease) underwent double IFTs, which indicated potentially unnecessary IFTs. These issues can be mitigated through the initial delivery of patients to the most appropriate facilities, facilitated by improved communication and medical information sharing among medical personnel and patientsвҖҷfamilies (14,17). The 2 parties should discuss IFT-related risks, which seem to be underestimated often. Additionally, after such IFTs, almost all patients underwent repeated laboratory or imaging tests, leading to increased medical costs, waste of healthcare resources, and an elevated radiation hazard in pediatric patients (18,19). The proportion of preventable IFTs in pediatric patients ranged from 19% to 39% worldwide (10,20-22). However, double IFTs were rarely reported in 0%-3.1% of pediatric patients who underwent IFTs (6,23), contrasting with the rate of 18.2% observed in South Korea.
In our study, we observed that the patients undergoing double IFTs stayed longer in the EDs, with nearly one-tenths of those having stayed in the EDs for longer than 12 hours. ED capacity is limited, and the extended EDLOS related to double IFT poses both individual and societal challenges, which are exacerbated by the current shortage of pediatric emergency resources, thus limiting other patientsвҖҷ opportunities to receive appropriate care. Managing the flow of IFT may offer a solution to pediatric ED overcrowding and optimize the use of the resources (24). This can be achieved by implementing a protocolized process, facilitating effective communication through a public coordinator, and using an electronic resource availability system.
Our study demonstrated that the reasons for IFTs varied depending on the initial ED visit. Unavailable medical resource was the most common reason for IFT in disease cases, and could be mitigated through more accurate IFT arrangements from the initial EDs (24). In contrast, the most common reason for injury cases was guardianвҖҷs request. Several factors contribute to such injury-related requests. In our study, the most frequent ED injury diagnosis was fracture of the upper extremity. A previous U.S. study reported that orthopedic problems in the hands were the most common ED diagnosis when the patients were discharged directly at the receiving EDs, suggesting that IFT is not always urgent or necessary (6). This difference in ED disposition between the U.S. and South Korea may be influenced by various factors. In South Korea, such factors may be a cultural preference for hospitalization, strong requests from guardians, lower healthcare costs, and the presence of private insurance systems. Therefore, policymakers and healthcare planners should consider developing targeted interventions to avoid redundant IFTs. These interventions could involve educational or administrative campaigns for the public, strengthening the national coordinating service for IFTs from EDs (24).
This study has several limitations. First, the NEDIS data did not provide detailed clinical information on the first medical facility visited and post-IFT outcomes in a sequential order. Thus, we could not determine the reason for the index IFT in the double-transfer group. In addition, there may be duplicates between the single- and double-transfer groups, or between only 2 IFTs and 3 or more IFTs in the latter group. Second, our study relied on KTAS and primary diagnosis codes assigned at ED discharge. These parameters do not fully reflect the severity of illness, and the coding sequences may vary among hospitals and personnel in charge, leading to inter- and intra-rater variability. Third, our study used national data from South Korea, and ED use patterns can vary across countries and healthcare systems. Lastly, we did not include patients who presented to local emergency medical institutes other than regional or local EMCs. However, the predominant disease in patients undergoing IFTs showed similarities with previous U.S. studies, and suggested the generalizability of the characteristics among these patients (6,10).
In summary, the prevalence of double IFTs in pediatric patients is noteworthy, and places a strain on medical resources, irrespective of the medical severity. The large number of double IFTs may be driven by guardiansвҖҷrequests rather than immediate medical necessity. This finding underscores the importance of raising awareness among the patientsвҖҷ caregivers about proper utilization of the pediatric emergency care system and strengthening the national coordinating service for IFTs.
NotesFunding sources This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant no. HR20C0026). Author contributions Conceptualization, Formal analysis, Funding acquisition, Software, Supervision, and Validation: YJ Kim Data curation: S Ahn and WY Kim Investigation: All authors Methodology and Visualization: MJ Kim Project administration and Resources: WY Kim Writing-original draft: MJ Kim and YJ Kim Writing-review and editing: All authors All authors read and approved the final manuscript. Fig.В 1.Flowchart outlining the selection of the study population. Levels I and II refer to regional and local emergency medical centers in South Korea, respectively. ED: emergency department. 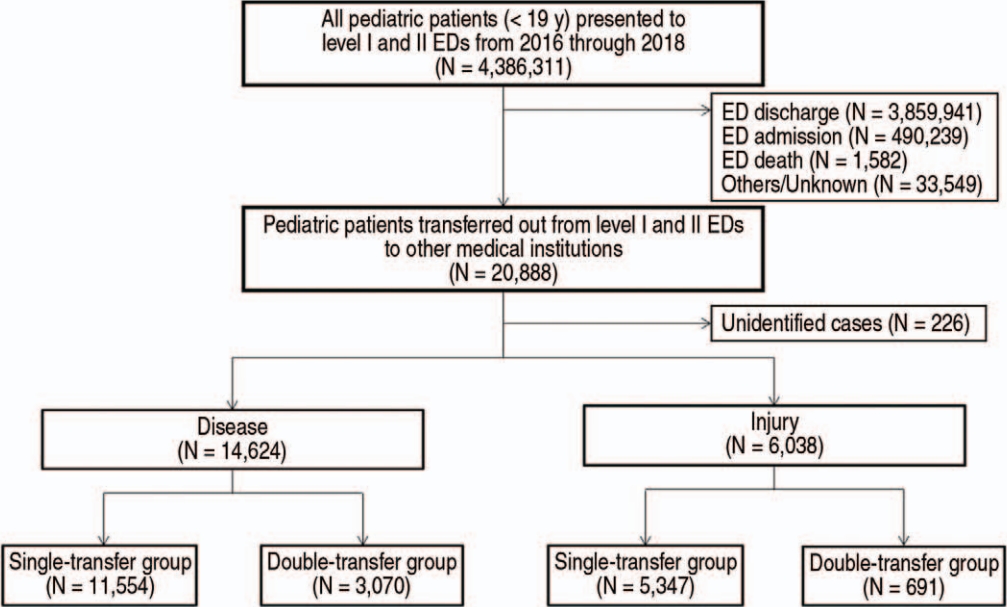
TableВ 1.Comparison of the characteristics between the single- and double-transfer groups
TableВ 2.ED utilization pattern
TableВ 3.Most common emergency department diagnoses and receiving institutions according to disease diagnoses
TableВ 4.Most common emergency department diagnoses and receiving institutions according to injury diagnoses
References1. American Academy of Pediatrics, Committee on Pediatric Emergency Medicine, American College of Emergency Physicians, Pediatric Committee, Emergency Nurses Association, Pediatric Committee. Joint policy statement--guidelines for care of children in the emergency department. J Emerg Nurs 2013;39:116вҖ“31.
2. Basco WT, Rimsza ME, Committee on Pediatric Workforce, American Academy of Pediatrics. Pediatrician workforce policy statement. Pediatrics 2013;132:390вҖ“7.
3. Bennett CL, Espinola JA, Sullivan AF, Boggs KM, Clay CE, Lee MO, et al. Evaluation of the 2020 pediatric emergency physician workforce in the US. JAMA Netw Open 2021;4:e2110084.
4. Schmitz GR. addressing shortages in pediatric emergency care-the evolution of health care access. JAMA Netw Open 2021;4:e2110115.
5. Cushing AM, Bucholz E, Michelson KA. Trends in regionalization of emergency care for common pediatric conditions. Pediatrics 2020;145:e20192989.
6. Li J, Monuteaux MC, Bachur RG. Interfacility transfers of noncritically ill children to academic pediatric emergency departments. Pediatrics 2012;130:83вҖ“92.
7. Huff AN, Keeperman JB, Osborn L. Chapter 74. Interfacility transportation. In: Cone DC, Brice JH, Delbridge TR, Myers JB, editors. Emergency medical services: clinical practice and systems oversight. 3rd ed. John Wiley & Sons, Inc.; 2021. p. 50-7.
8. Hernandez-Boussard T, Davies S, McDonald K, Wang NE. Interhospital facility transfers in the United States: a nationwide outcomes study. J Patient Saf 2017;13:187вҖ“91.
9. Mueller S, Zheng J, Orav EJ, Schnipper JL. Interhospital transfer and patient outcomes: a retrospective cohort study. BMJ Qual Saf 2019;28:e1.
10. Mohr NM, Harland KK, Shane DM, Miller SL, Torner JC. Potentially avoidable pediatric interfacility transfer is a costly burden for rural families: a cohort study. Acad Emerg Med 2016;23:885вҖ“94.
11. Golestanian E, Scruggs JE, Gangnon RE, Mak RP, Wood KE. Effect of interhospital transfer on resource utilization and outcomes at a tertiary care referral center. Crit Care Med 2007;35:1470вҖ“6.
12. Barry PW, Ralston C. Adverse events occurring during interhospital transfer of the critically ill. Arch Dis Child 1994;71:8вҖ“11.
13. Chaichotjinda K, Chantra M, Pandee U. Assessment of interhospital transport care for pediatric patients. Clin Exp Pediatr 2020;63:184вҖ“8.
14. Kim YJ, Hong JS, Hong SI, Kim JS, Seo DW, Ahn R, et al. the prevalence and emergency department utilization of patients who underwent single and double inter-hospital transfers in the emergency department: a nationwide population-based study in Korea, 2016-2018. J Korean Med Sci 2021;36:e172.
15. Lim T, Park J, Je S. Pediatric Korean Triage and Acuity Scale. Pediatr Emerg Med J 2015;2:53вҖ“8. Korean.
16. Han KS, Jeong J, Kang H, Kim WY, Kim SJ, Lee SW. Association between the emergency department length of stay time and in-hospital mortality according to 28 diagnosis groups in patients with severe illness diagnosis codes. J Korean Soc Emerg Med 2021;32:77вҖ“88. Korean.
17. Nacht J, Macht M, Ginde AA. Interhospital transfers from U.S. emergency departments: implications for resource utilization, patient safety, and regionalization. Acad Emerg Med 2013;20:888вҖ“93.
18. Kocher KE, Meurer WJ, Desmond JS, Nallamothu BK. Effect of testing and treatment on emergency department length of stay using a national database. Acad Emerg Med 2012;19:525вҖ“34.
19. Gupta R, Greer SE, Martin ED. Inefficiencies in a rural trauma system: the burden of repeat imaging in interfacility transfers. J Trauma 2010;69:253вҖ“5.
20. Fenton SJ, Lee JH, Stevens AM, Kimbal KC, Zhang C, Presson AP, et al. Preventable transfers in pediatric trauma: a 10-year experience at a level I pediatric trauma center. J Pediatr Surg 2016;51:645вҖ“8.
21. Peebles ER, Miller MR, Lynch TP, Tijssen JA. Factors associated with discharge home after transfer to a pediatric emergency department. Pediatr Emerg Care 2018;34:650вҖ“5.
22. Lieng MK, Marcin JP, Dayal P, Tancredi DJ, Swanson MB, Haynes SC, et al. Emergency department pediatric readiness and potentially avoidable transfers. J Pediatr 2021;236:229вҖ“237.e5.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

 |
 |