 |
 |
AbstractIliopsoas abscess (IPA) rarely occurs in newborns and infants. Symptom triad, including fever, inguinal swelling or discoloration, and limited lower limb movement, is observed in most cases. Herein, we report a case of unusual IPA in an 82-day-old boy who presented with fever as the only symptom. To our best knowledge, there have been no reports of infant IPA presenting without localizing signs. This report highlights the importance of a high degree of suspicion for timely diagnosis of infant IPA when an infant presents only with fever.
IntroductionIliopsoas abscess (IPA), a collection of pus involving the iliopsoas muscle, is a rare disease in neonates and infants (1). Owing to its rarity, a high index of suspicion is important for timely diagnosis and treatment (2-4). The 3 most common symptoms of neonatal IPA are fever, inguinal swelling or discoloration, and limited lower limb movement (3,5-7). If the symptom triad is present, ultrasonogram (US), computed tomography, or magnetic resonance imaging (MRI) should be performed to diagnose IPA (3).
We present a case of IPA in an 82-day-old boy who presented with fever without localizing signs and was initially hospitalized for presumptive diagnosis of urinary tract infection (UTI). This study was approved by the institutional review board at Hanyang University Hospital with a waiver for informed consent (IRB no. 2023-06-039).
CaseAn 82-day-old boy visited the emergency department (ED) with fever lasting for 3 days as the only symptom. Initial vital signs were as follows: heart rate, 160 beats/minute; respiration rate, 40 breaths/minute; and temperature, 38.1 ℃. No abnormalities were found in physical and neurological examinations. He was delivered by elective cesarean section at a gestational age of 38 weeks with a birth weight of 3,000 g. His mother had no relevant medical history at the time of delivery. Laboratory findings showed a white blood cell count of 27.4 × 103/µL with 64.3% segmented neutrophils and C-reactive protein concentration of 15.7 mg/dL. Urinalysis, which used the urine collected with a urine bag, showed 5-9 cells/high-power field. The boy was hospitalized to treat UTI as a presumptive diagnosis and given cefotaxime.
After hospitalization, 50,000 colony-forming units/mL of Streptococcus agalactiae, which was susceptible to cefotaxime, were identified in the urine. Despite the absence of pyuria on a follow-up urine and antibiotic therapy, fever persisted until day 3. An abdominal US was performed to evaluate the cause of the fever, showing a 3.1 cm-sized hypoechoic lesion occupying the left pelvis (Fig. 1). On the same day, an MRI suggested that the pelvic mass was a left IPA (Fig. 2). Considering the imaging finding, vancomycin was added to cover a possible involvement of Staphylococcus aureus, the most commonly identified pathogen in IPA (1,4,8-10). On day 4, we inserted a pigtail catheter for percutaneous drainage and immediately drained 5 mL of thick purulent pus. On day 6, blood culture was found to be negative, and the fever subsided.
On day 7, a follow-up US showed a decrease in the size of IPA. Methicillin-sensitive S. aureus was isolated with the drained pus. On day 11, the draining catheter was removed. On day 14, the follow-up laboratory findings showed a white blood cell count of 11.9 × 103/µL and C-reactive protein concentration of < 0.3 mg/dL. On the same day, the boy was discharged uneventfully. He had been well without any symptoms until 15-month follow-up.
DiscussionOwing to its rarity in infants, IPA is seldom suspected as a differential diagnosis at the initial presentation (2,7). In 2014, the first case of neonatal IPA was reported in Korea, and approximately 20 cases of neonatal IPA have been reported in English literature (1). Imaging tests, including US, computed tomography, and MRI, are performed to detect IPA if the infant has the abovementioned symptom triad. In the present case, there were no symptoms other than fever. Thus, it was difficult to suspect IPA at the ED. UTI was initially suspected given the initial pyuria, and later S. agalactiae were found in the urine. However, the persistent fever prompted performing US. The US showed the pelvic mass, which was confirmed as IPA on MRI. Based on the MRI findings and pus culture, we consider that the infant boy had a primary IPA due to methicillin-sensitive S. aureus with secondary UTI, which was developed by extrinsic compression of the urinary bladder. After the surgical drainage and broad-spectrum antibiotic therapy, he was discharged uneventfully.
Our case is unique because the infant boy had no localized groin symptoms, which have been reported in previous literature (1-7,9-13). To our best knowledge, most literature regarding neonatal IPAs shows that patients consistently had localizing signs, such as inguinal swelling or discoloration (1-7,9-13). The localized signs of IPA develop when the abscess spreads inferiorly to the inguinal area (14). However, reviewing the MRI findings (Fig. 2), the abscess was extending into the pelvic cavity, rather than spreading inferiorly. We assume that the location of the IPA might have resulted in the absence of groin symptoms.
Regarding treatment, antibiotic therapy alone is usually insufficient, and surgical drainage is needed in most cases (2,4,5,7,10). In the present case, the fever persisted despite the antibiotic therapy during the first 3 days. If the imaging tests had not been performed, the detection of IPA would have been delayed, predisposing the infant boy to complications, such as sepsis (2,9). For early detection and appropriate treatment, the possibility of IPA should be considered in infants presenting with intractable fever without localizing signs.
Neonatal or infant IPA is a rare disease difficult to diagnose without the symptom triad (7). The present case suggests that IPA can occur in young infants without the classic inguinal swelling or discoloration. Infants having fever without localizing signs frequently undergo physical examination, laboratory tests, urinalysis, blood culture, or cerebrospinal fluid profile in EDs. If these tests do not identify the cause of fever, or if the fever persists despite the antibiotic therapy, additional imaging tests should be promptly performed to find IPA.
NotesFig. 1.Abdominal ultrasonogram on day 3. It shows a 3.1 cm-sized hypoechoic lesion occupying the left pelvis. 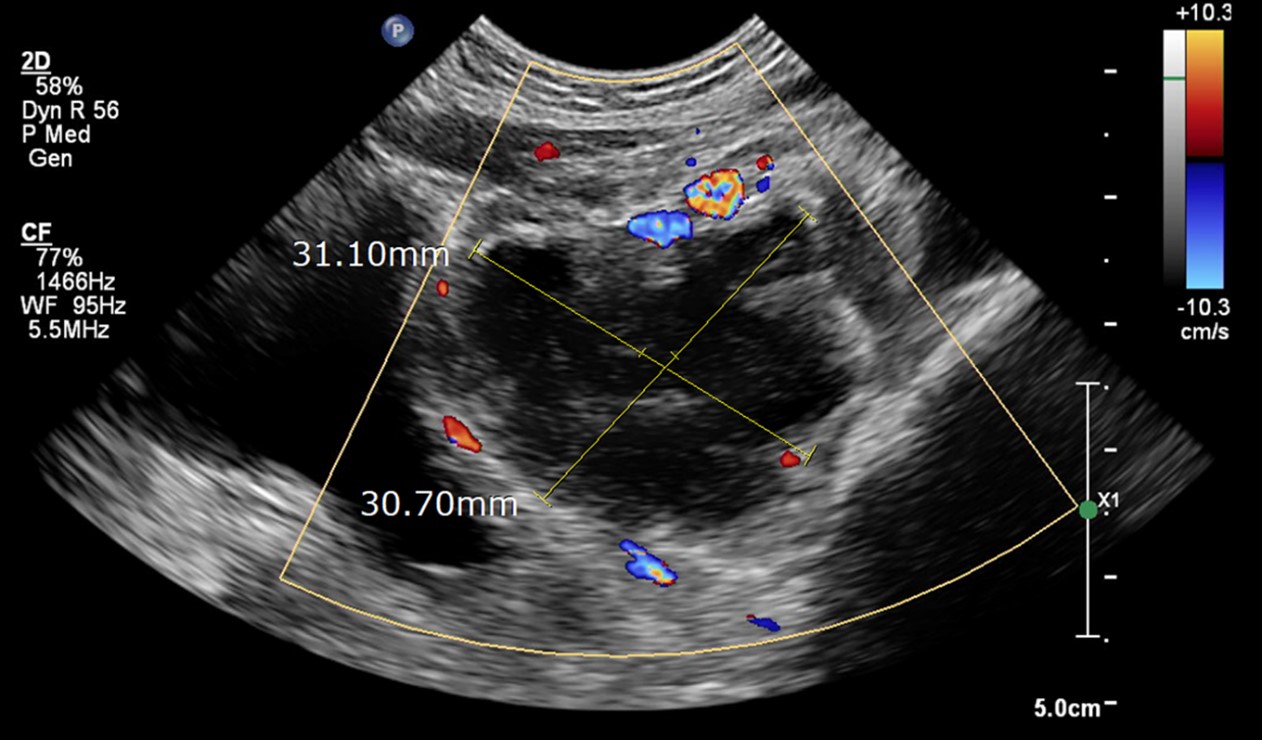
Fig. 2.Pelvic magnetic resonance imaging on day 3. Axial scans show a 3.4 cm-sized peripheral enhancing mass involving the left iliopsoas muscle (arrow, A [T1-weighted image]) and right-sided deviation of the rectum and bladder (arrowheads, B [T2-weighted image]). The mass is also noted on coronal scan (arrowheads, C [T2]). 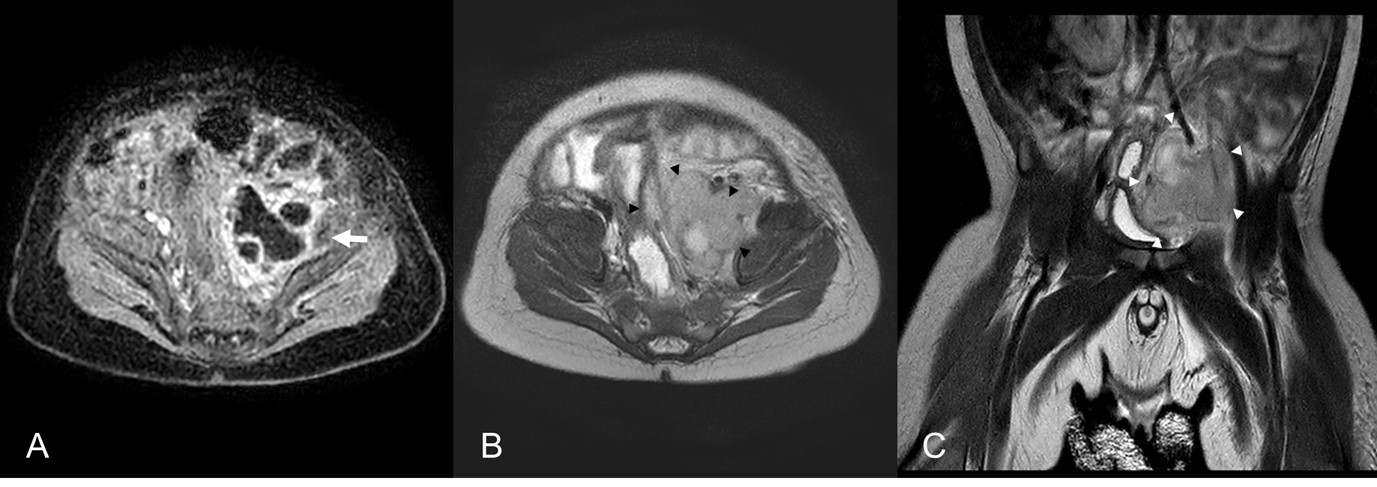
References1. Han YM, Kim AY, Lim RK, Park KH, Byun SY, Kim SH, et al. Neonatal iliopsoas abscess: the first Korean case. J Korean Med Sci 2015;30:1203–6.
2. Ray S, Dey PK, Halder P, Ghosh A. Diagnostic dilemma of primary neonatal iliopsoas abscess. Ann Pediatr Surg 2021;17:30.
3. Venkatesan DK, Chaudhary H, Verma S. Every loin swelling in an infant is not a renal mass: rare presentation of psoas abscess in an infant. BMJ Case Rep 2020;13:e237137.
4. Akin MS, Agackiran D, Unal E, Yavuz OO, Yigit S. Neonatal iliopsoas abscess presenting with transient cyanosis of a single extremity: a case report and review of the literature. Turk J Pediatr 2020;62:160–4.
5. Yano T, Takamatsu H, Noguchi H, Tahara H, Kaji T, Saruwatari Y, et al. Iliopsoas abscess in the neonate. J Pediatr Surg 2004;39:e13–5.
7. Ishibashi H, Oshio T, Sogami T, Nii A, Mori H, Yada K, et al. Iliopsoas abscess in an infant. J Med Invest 2014;61:213–6.
8. Lopez VN, Ramos JM, Meseguer V, Perez Arellano JL, Serrano R, Ordonez MA, et al. Microbiology and outcome of iliopsoas abscess in 124 patients. Medicine (Baltimore) 2009;88:120–30.
9. Saeed M, Shirazi IH. A rare case report of neonatal iliopsoas abscess presenting as swelling of left hip. J Pak Med Assoc 2020;70:2467–8.
10. Wang E, Ma L, Edmonds EW, Zhao Q, Zhang L, Ji S. Psoas abscess with associated septic arthritis of the hip in infants. J Pediatr Surg 2010;45:2440–3.
11. Horiuchi A, Kameoka K, Kuwabara J, Watanabe Y, Kawakami S, Tauchi H, et al. Neonatal iliopsoas abscess. Pediatr Int 2012;54:712–4.
12. Nisar MU, Sikander S, Noorain Z, Baig MS, Akhtar N. Primary iliopsoas abscess in a neonate. J Coll Physicians Surg Pak 2019;29:S45–7.
|
|
|||||||||||||||||||||||||||||||||||

 |
 |