 |
 |
AbstractNeonatal tension pneumothorax is life-threatening. A tension pneumothorax on the right side was detected on a newborn boy weighing 2,380 g, who was born at 35 weeks of gestation. Given the unavailability of an on-duty thoracic surgeon and appropriately sized chest tubes in the neonatal intensive care unit, an emergency physician performed closed thoracostomy using two 7-French latex catheters. Immediately after the re-expansion of the right lung, left tension pneumothorax was newly detected. Two more 7-French latex catheters were inserted, relieving the left lesion. We consider that the right pneumothorax occurred due to the mixture of spontaneous rupture of the subpleural blebs and barotrauma during the initial positive pressure ventilation, while the left lesion did due to the high-flow oscillatory ventilation. Despite the limited availability of devices in the present case, a favorable outcome was achieved by the use of alternative catheters, which were chosen by the emergency physician.
IntroductionNeonatal tension pneumothorax is life-threatening, and requires immediate needle and/or tube thoracostomy1). According to a Danish study performed on 71 neonates with pneumothorax, median onset of the pneumothorax was 28.5 hours in preterm neonates (c.f., 6.1 hours in term)2). Herein, we report a preterm low-birth-weight newborn with bilateral tension pneumothoraces, which were successfully decompressed using latex catheters by an emergency physician (EP). This study was approved by the institutional review board of CHA Gumi Medical Center with a waiver for informed consent (IRB no. GM20-03).
CaseA newborn boy weighing 2,380 g was born to a 26-year-old mother via cesarean section, which was performed due to a sudden deceleration of fetal heart rate to 80 beats/minute, after 35 weeks of gestation. The mother had no health problems during her pregnancy, and received regular antenatal care till the term. Initially, the newborn appeared slightly cyanotic with pale skin. The sequentially measured Apgar scores were 3, 5, 6, and 7, at 1, 5, 10, and 15 minutes of life, respectively. The initial vital signs at 5 minutes of life were blood pressure, 65/35 mmHg; heart rate, 146 beats/minute; respiratory rate, 76 breaths/minute; and oxygen saturation, 91% on room air.
A few minutes later, the newborn’s heart rate decreased to 100 beats/minute, and promptly a positive pressure ventilation was applied. On the right side, breathing sounds decreased with the positive transillumination. Immediate needle thoracostomy was performed by a neonatologist given the clinical suspicion of tension pneumothorax. Even following the procedure, the heart rate remained at 100-110 beats/minute. Thus, endotracheal intubation was performed in the delivery room. No obvious meconium staining was seen on the laryngoscopic view. The newborn was transferred to the neonatal intensive care unit (NICU).
At the NICU, high-flow oscillatory ventilation was started. The initial radiograph showed a right-sided pneumothorax with the trachea and heart shifted to the left side (Fig. 1). Given the unavailability of an on-duty thoracic surgeon, an attending EP was called to the NICU for tube thoracostomy. The NICU was not stocking appropriately sized chest tubes or catheters, such as a trocar or polyurethane catheter. Thus, a 7-French (Fr) latex catheter (Latex Nelaton Catheter; Sewoon Medical Co. Ltd., Cheonan, Korea) was inserted through the fourth intercostal space (ICS) following the creation of the extra side holes on the catheter (Fig. 2). More than 200 mL of air was manually drained through the catheter. An underwater seal drainage was set up afterward. Notably, the skin color become more pinkish, but remained pale with a PaO2 of 74 mmHg. Despite continuous air flow from the catheter for 30 minutes following the drain placement, breathing sounds remained decreased on the right side with a residual pneumothorax on a repeat radiograph. Although the EP repositioned the catheter and gently applied a - 5 cmH2O pressure suctioning, the pneumothorax failed to resolve. At this point, the second catheter of the same type and size was placed through the right seventh ICS, with subsequent reexpansion of the right lung confirmed on a followup radiograph.
However, a newly developed, left pneumothorax was detected with total lung collapse (Fig. 3). Accordingly, another 7-Fr latex catheter (third) was promptly inserted through the left fourth ICS. A follow-up radiograph showed the mediastinum shifted to the right side despite the appropriately positioned, third catheter. A few minutes later, left breathing sounds remained decreased with a PaO2 of 67 mmHg, despite a continuous air evacuation via the third catheter. The fourth 7-Fr latex catheter was placed through the left sixth ICS, and resultantly, the left lung was expanded (Fig. 4). The newborn was successfully weaned from the mechanical ventilation and extubated on day 7, and discharged uneventfully on day 11.
DiscussionIn this case, the right tension pneumothorax occurred presumably due to the mixture of spontaneous rupture of the subpleural blebs and barotrauma during the initial positive pressure ventilation, while the left lesion did due to the highflow oscillatory ventilation. Respiratory distress syndrome, transient tachypnea in newborn, and meconium aspiration syndrome were excluded given the gestational age and radiologic or laryngoscopic findings.
Close observation with oxygen administration may be appropriate for hemodynamically stable neonates with small-volume pneumothorax. According to previous studies, 33.3%-71.1% of neonatal pneumothoraces were treated without invasive procedures 2-4). In cases of large-volume pneumothorax, chest drain placement is advised for decompression. Tube thoracostomy is the traditional method of choice, similar to that of older children. Compared to chest tubes, pigtail and venous catheters are technically easier to insert, supporting the catheters as a safe and effective alternative to chest tubes5-7). Also, small-caliber latex catheters can be chosen in neonatal pneumothorax8). Prompt recognition and intervention is required in cases of tension pneumothorax, as in the present case. Immediate needle thoracostomy should be performed as the initial step. If the needle thoracostomy is insufficient for decompression, tube thoracostomy should be followed. Despite the unavailability of the on-duty thoracic surgeon and appropriately sized chest tubes, the EP troubleshot with a total of four 7-Fr latex catheters.
In conclusion, neonatal bilateral tension pneumothoraces require prompt tube thoracostomy. The circumstantial limitations in the present case were overcome by the EP’s decisions on prompt and sequential use of effective alternatives to chest tubes.
Fig. 1.Large-volume tension pneumothorax on the right side. Note the total collapse of the right lung with the mediastinal shift. An endotracheal tube is inserted. 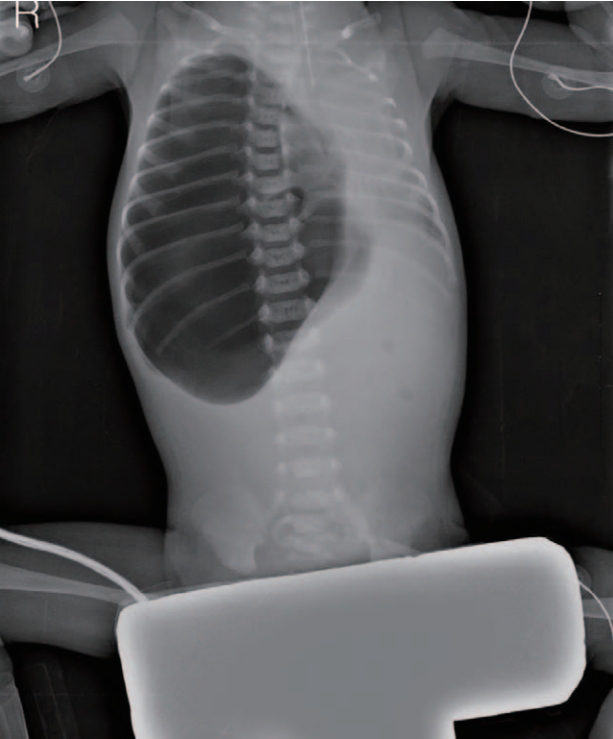
Fig. 2.Insertion of the first, 7-French latex catheter (“1”). Volume of the tension pneumothorax remains despite the insertion. 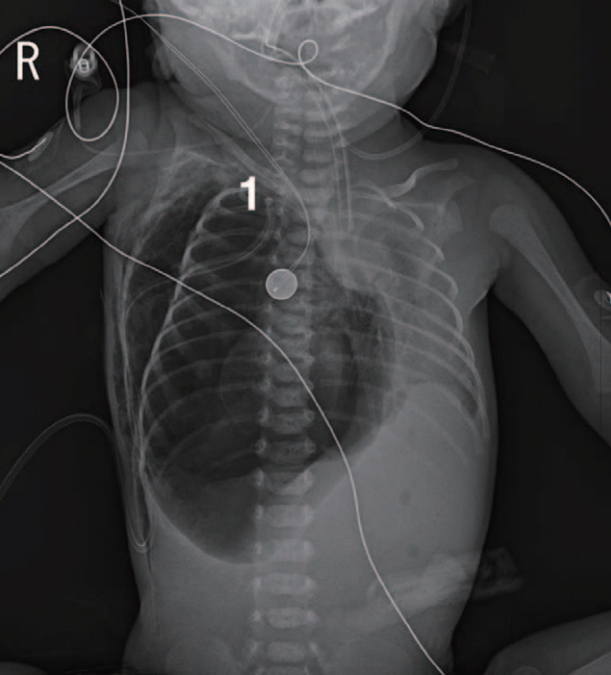
References1. Kim SK, Kim WH. Tension pneumothorax in a newborn after Cesarean-section delivery: a case report. Korean J Anesthesiol 2010;59:420–4.
2. Vibede L, Vibede E, Bendtsen M, Pedersen L, Ebbesen F. Neonatal pneumothorax: a descriptive regional Danish study. Neonatology 2017;111:303–8.
3. Smith J, Schumacher RE, Donn SM, Sarkar S. Clinical course of symptomatic spontaneous pneumothorax in term and late preterm newborns: report from a large cohort. Am J Perinatol 2011;28:163–8.
4. Kim EA, Jung JH, Lee SY, Park SH, Kim JS. Neonatal pneumothorax in late preterm and full-term newborns with respiratory distress: a single-center experience. Neonatal Med 2022;29:18–27.
5. Panza R, Prontera G, Ives KN, Zivanovic S, Roehr CC, Quercia M, et al. Pigtail catheters versus traditional chest drains for pneumothorax treatment in two NICUs. Eur J Pediatr 2020;179:73–9.
6. Arda IS, Gürakan B, Alíefendío˘glu D, Tüzün M. Treatment of pneumothorax in newborns: use of venous catheter versus chest tube. Pediatr Int 2002;44:78–82.
7. Bruschettini M, Romantsik O, Ramenghi LA, Zappettini S, O’Donnell CP, Calevo MG. Needle aspiration versus intercostal tube drainage for pneumothorax in the newborn. Cochrane Database Syst Rev 2016;CD011724.
8. Liu J, Cao HY, Sorantin E. Pneumothorax of the newborn. In: Liu J, Cao HY, Sorantin E, editors. Neonatal lung ultrasonography. Dordrecht: Springer Nature; 2018. p. 111-22.
|
|
|||||||||||||||||||||||||||||||||||

 |
 |