A study on the characteristics of patients visiting the pediatric emergency department with post-tonsillectomy hemorrhage
Article information
Abstract
Purpose
This study was performed to identify risk factors associated with post-tonsillectomy hemorrhage (PTH)-related hospitalization in pediatric patients visiting an emergency department (ED).
Methods
We retrospectively reviewed the medical records of patients who underwent tonsillectomy at a single children’s hospital ED from January 2009 through December 2020. Data were collected on patient demographics, chief complaints, surgical methods, postoperative days, initial vital signs, and laboratory findings. The study population was divided into hospitalized and discharged groups.
Results
Among a total of 2,716 patients reviewed, 67 met the inclusion criteria. The hospitalized group showed a lower median systolic blood pressure (108.0 [interquartile range, 82.0-134.0] vs. 118.5 [89.8-147.2] mmHg; P = 0.021) and a faster median respiratory rate (23.0 [18.0-28.0] vs. 20.0 [17.0-23.0] breaths/minute; P = 0.019), compared with the discharged group. Multivariable logistic regression identified systolic blood pressure under 100 mmHg (odds ratio, 5.21; 95% confidence interval, 1.17-37.60) and respiratory rate over 24 breaths/minute (7.31; 1.07-145.79) as the factors associated with PTH-related hospitalization.
Conclusion
When pediatric patients visit EDs for PTH, close monitoring or hospitalization may be needed in those with low systolic blood pressure or rapid respiratory rate.
Introduction
Tonsillectomy is a common surgical procedure performed in pediatric patients, indicated for recurrent throat infections and obstructive sleep apnea (1,2). Its postoperative complications include airway obstruction, laryngospasm, airway edema, bronchospasm, hemorrhage, dehydration, infection, velopharyngeal insufficiency, and nasopharyngeal stenosis (2,3). Post-tonsillectomy hemorrhage (PTH) is a leading cause of death that may occur at any time in the postoperative period occurring at a rate of 0.28%-20% (4,5). During tonsillectomy, ligation or cauterization is performed on multiple arteries perfusing to the palatine tonsils, which originate from the external carotid arteries and tonsillar venous plexus. The surgery also involves dissecting the tonsils and their capsules from the muscle wall and removing them from the peritonsillar space, and can lead to fatal hemorrhage (2).
Nowadays, most of the surgeries are performed on the same day, thus postoperative management is conducted in primary care clinics or emergency departments (EDs) rather than on an inpatient basis (2,6). Thus, emergency physicians should know the characteristics of patients visiting EDs with PTH and the factors associated with PTH-related hospitalization. However, most relevant studies on factors associated with PTH have been conducted in outpatient departments of otorhinolaryngology rather than in EDs (7-13). Therefore, we conducted a study to identify factors associated with PTH-related hospitalization in pediatric patients visiting the ED.
Methods
We retrospectively reviewed the medical records of 2,716 patients who underwent tonsillectomy or adenoidectomy at Seoul National University Children’s Hospital, a tertiary center in Seoul, Republic of Korea, from January 2009 through December 2020. We included patients younger than 18 years who visited the pediatric ED with chief complaints of bleeding-related symptoms within 30 days of tonsillectomy or adenoidectomy performed at the same hospital. The surgery was performed by several otolaryngologists. Exclusion criterion was a symptom not related to surgery or bleeding.
The data of interest included baseline characteristics, chief complaints, initial vital signs, concentrations of hemoglobin and platelet, postoperative days, and type of surgery. Chief complaints included operation site bleeding, bloody vomiting, epistaxis, bloody sputum, and others. The study population was divided into hospitalized and discharged groups. The study protocol was approved by the institutional review board of the Seoul National University Hospital with a waiver for informed consent (IRB no. 2010-171-1169).
In the univariable analysis stage, we checked the variables for normality and expected frequencies and used the Mann-Whitney and Fisher’s tests. Variables with P < 0.05 in univariable analyses were put into a multivariable logistic regression model. For the multivariable analysis, continuous variables were dichotomized using the random forest technique. For a variable significantly associated with a high risk by the multivariable analysis, the odds ratio was calculated with the corresponding 95% confidence interval. All statistical analyses were performed using R Statistical Software (ver. 4.1.1; R Foundation for Statistical Computing).
Results
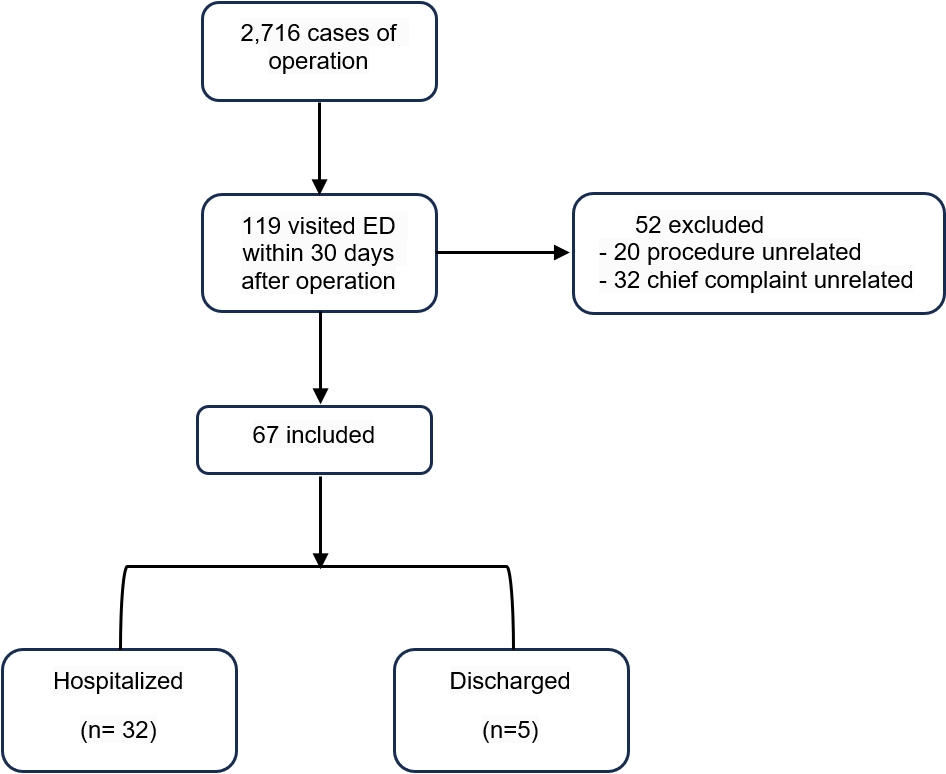
Among a total of 2,716 patients undergoing tonsillectomies during the study period, 119 visited the ED within 30 days after the surgeries. Among them, 52 patients were excluded, leaving the study population of 67 patients (Fig. 1).
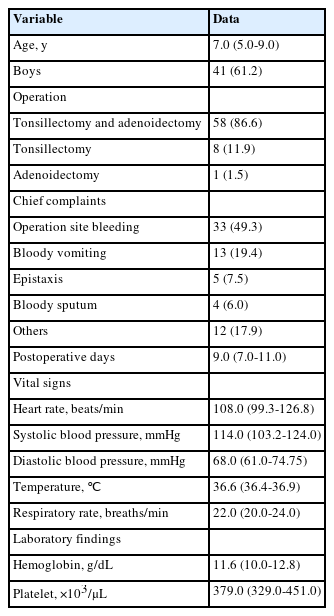
These 67 patients consisted of 41 boys (61.2%) and 26 girls (38.8%), with a median age of 7.0 years (interquartile range, 5.0-9.0) (Table 1). Fifty-eight patients (86.6%) underwent both tonsillectomy and adenoidectomy, 8 (11.9%) did tonsillectomy only, and 1 (1.5%) did adenoidectomy only. Operation site bleeding was the most common chief complaint.
Of the 67 patients, 32 (47.8%) were hospitalized (Table 2). The hospitalized group had a lower systolic blood pressure (median value, 108.0 vs. 118.5 mmHg; P = 0.021) and a faster respiratory rate (23.0 vs. 20.0 breaths/minute; P = 0.019) than the discharged group. However, no significant difference was observed in the other factors.
As a result of the logistic regression, systolic blood pressure under 100 mmHg (odds ratio, 5.21; 95% confidence interval, 1.17-37.60; P = 0.023) and respiratory rate over 24 breaths/minute (7.31; 1.07-145.79; P = 0.049) were independently associated with hospitalization (Table 3).
In the hospitalized patients, 3 (4.5%) underwent bleeding control surgeries, 10 (14.9%) received transfusion, 13 (19.4%) received fluid replacement, and 18 (26.9%) were discharged after only observation as their diet progressed smoothly. No in-hospital mortality occurred.
Discussion
In this study, we found that hypotension and tachypnea may increase the risk of hospitalization when visiting the ED for PTH.
Steketee and Reisdorff (13) studied 106 patients of all ages with PTH who visited an ED. Of the 61 pediatric patients, 21 showed tachycardia or hypotension. However, the statistical association of the vital signs could not be investigated due to incomplete records. Likewise, in our study, hypotension was significantly associated with PTH-related hospitalization.
In addition, we found an association between tachypnea and hospitalization. Peterson and Losek (14) studied 90 patients who visited an ED due to PTH that occurred 24 hours after the tonsillectomy or later, and reported tachypnea and tachycardia suggestive of compensated shock in 4.4% (4 of the 90 pediatric patients). As we speculate, the abnormal vital signs are thought to be due to dehydration, poor oral intake, as well as hemorrhage per se, and are common post-tonsillectomy complications in children.
In our study, there were no significant differences in sex, age, type of operation, or postoperative day. Although some studies have reported a relationship between age and PTH (5,9), there is still no consensus in the literature on age as a risk factor for PTH (6). Similar to our results, Susaman et al. (10) reported that age had no significant differences in PTH.
Our study has several limitations. First, it was conducted in a single center with a small sample size. Second, the analysis was limited due to missing values in the laboratory variables. Missing values were observed only in the discharged group, suggesting that the emergency physicians had already decided whether to perform the tests. Third, there may be patients who did not visit the ED even if there was postoperative bleeding. Fourth, we did not consider the interrater reliability.
Nevertheless, from what we know, our research has some differences from other studies. First, to our knowledge, there have been few studies analyzing the association between vital signs and outcomes of PTH. Second, unlike otolaryngology-based studies, ours was performed at the ED. Third, unlike relevant studies, we sought to investigate factors for PTH-related hospitalization. ¬¬
When pediatric patients come to EDs for PTH, some should be closely monitored and considered for hospitalization, particularly those who show hypotension and tachypnea. Larger studies are needed to confirm the association between abnormal vital signs and PTH-related hospitalization.
Notes
Author contributions
Conceptualization, Methodology: all authors
Data curation, Formal analysis, Investigation, Project administration, Resources, Software, Validation, and Visualization: H Jang and EJ Lee
Supervision: EJ Lee
Writing-original draft: all authors
Writing-review and editing: H Jang, EJ Lee, and DK Kim
All authors read and approved the final manuscript.
Conflicts of interest
No potential conflicts of interest relevant to this article were reported.
Funding sources
No funding source relevant to this article was reported.
Data availability
Data cannot be opened to the public due to the privacy policy of institutional review board.