Profile of pediatric ophthalmic referrals in a single emergency department in Korea
Article information
Abstract
Purpose
This study was performed to examine a comprehensive profile of ophthalmic (OPH) referrals based on diagnosis in a single emergency department (ED) in Korea.
Methods
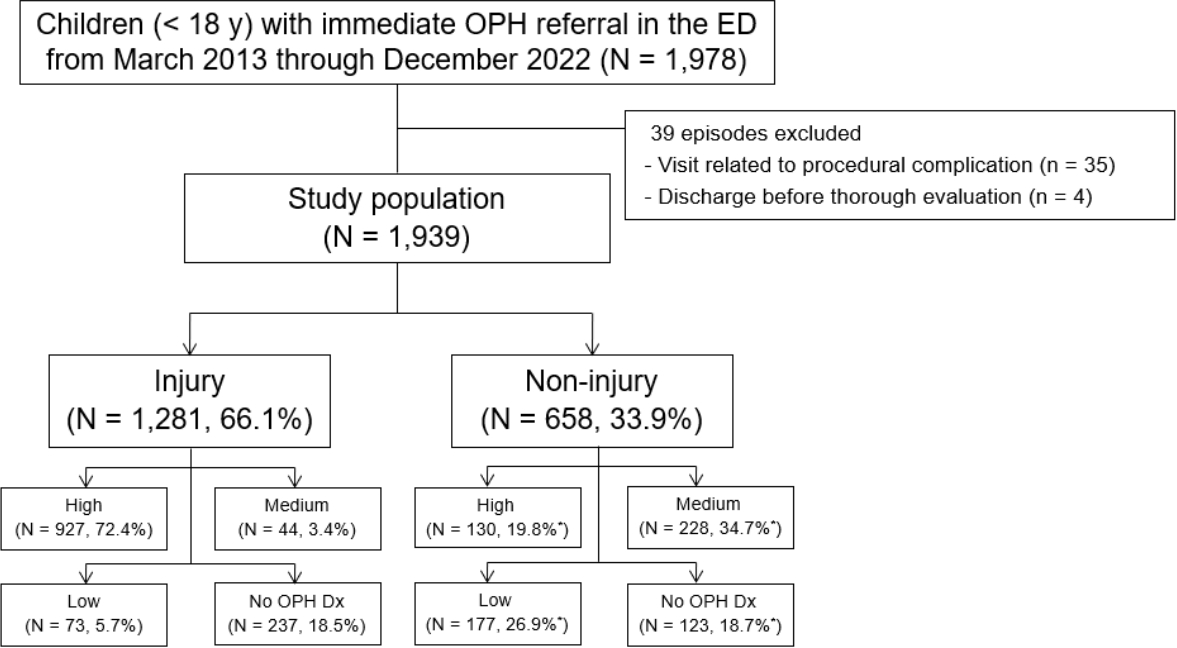
We analyzed the clinical profiles of children (< 18 years) who underwent immediate OPH referrals in a tertiary hospital ED, from March 2013 through December 2022. Exclusion criteria were a visit related to procedural complication and a discharge before thorough evaluation. We focused on a diagnosis-based high OPH severity requiring emergency surgery or hospitalization. The profiles were compared according to the severity and age group (0-3, 4-6, 7-12, and 13-17 years).
Results
A total of 1,939 children consisted of 1,281 (66.1%) with injury and 658 (33.9%) with non-injury. Top 3 injuries were orbital fracture, hyphema, and corneal abrasion, whereas top 3 non-injuries were keratoconjunctivitis, cellulitis, and hordeolum. Children with high OPH severity (54.5%) had significantly lower proportions of girls (26.5% vs. 38.9%), visits on weekend/holiday (34.4% vs. 43.4%), and most non-injury chief complaints, and higher proportions of 13-17 years (41.1% vs. 23.6%), injury (87.7% vs. 40.1%), emergency surgery (4.9% vs. 0.1%), in-ED procedure (9.3% vs. 2.4%), hospitalization (4.0% vs. 0.8%), and most injury mechanisms. With increasing age, high OPH severity, orbital fracture, and hyphema increased in proportions, in contrast to a decreasing tendency in corneal abrasion, keratoconjunctivitis, cellulitis, and hordeolum (all Ps for trend ≤ 0.001). There were 610 (31.5%) children with low OPH severity or no OPH diagnosis.
Conclusion
True OPH emergencies may be more common in injured, older, or male children. This finding could be useful in focusing on emergencies while diverting less urgent cases to outpatient departments or outside ophthalmology clinics.
Introduction
In emergency departments (EDs), children or adolescents (henceforth children, unless otherwise specified) with eye-related symptoms account for approximately 30% of patients of all ages with similar symptoms (1). This aligns with the pediatric proportion of emergency patients of all ages, falling within the range of 25%-35% (2). Furthermore, these symptoms pose a threat to vision or provoke medical concerns for children or their guardians, prompting visits to EDs. However, this demand for emergency ophthalmic (OPH) care often goes unmet due to challenges in recruiting on-call ophthalmologists and frequent non-emergency visits reaching 44.3%-49.4% (1,3,4). Under these circumstances, emergency physicians and pediatricians should focus on true OPH emergencies while discerning non-emergencies. We aimed to provide a comprehensive profile of OPH referrals in a single ED in Korea based on diagnosis.
Methods
1. Study design, setting, and population
This retrospective study was based on the medical records of children (< 18 years) who underwent immediate OPH referrals in a tertiary hospital ED, from March 2013 through December 2022. The ED cares for approximately 21,000 children annually and provides on-call ophthalmologist services on a 24/7 basis. For similar symptom-related return visits within 1 week of the index visit, we analyzed data from the first visit to guarantee the independence of the visits of the same child. Exclusion criteria were a visit related to procedural complication and a discharge before a thorough evaluation. This study was approved by the institutional review board of Ajou University School of Medicine with a waiver for informed consent (IRB no. AJOUIRB-DB-2023-321).
In the ED, children presenting with eye-related symptoms are initially evaluated by attending emergency physicians or residents who perform essential examinations, such as pupil or slit lamp. If needed, the physicians refer the children to on-call ophthalmologists. Subsequently, the ophthalmologists usually check the children’s visual acuity, intraocular pressure, slit lamp, pupil, ocular movement, and fundus in the listed order, using age-appropriate methods (5,6). Imaging tests are performed at the discretion of the ophthalmologists or emergency physicians.
2. Data collection
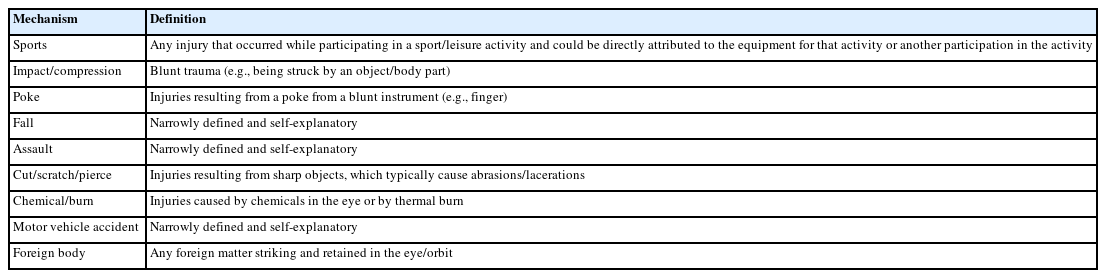
Variables of interest included age (years) with age groups (0-3 [infants-toddlers], 4-6 [preschoolers], 7-12 [schoolers], and 13-17 years [adolescents]), sex, time of visit (night [18:00-07:59], weekend/holiday, and seasons [March-May, June-August, September-November, and December-February]), ED-assigned Korean Triage and Acuity Scale (KTAS) (7), mechanism and place of injury, chief complaint (for non-injury cases), OPH or imaging tests, OPH diagnosis, emergency surgery or in-ED procedure (performed < 48 hours of visits), and hospitalization to Department of Ophthalmology. Injury mechanisms were broken down as per a study performed in the ED of Wills Eye Hospital in Philadelphia, PA (Appendix 1, https://doi.org/10.22470/pemj.2023.00843) (8). A KTAS 1-2 was considered high ED-assigned acuity (9). The places of injury were categorized as home, playground, road, educational facility, and public.
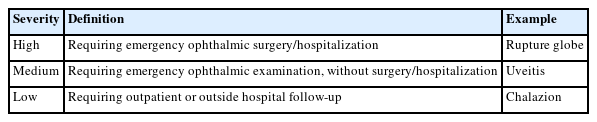
For OPH diagnosis, we chose the diagnoses made on the same days by on-call ophthalmologists over the final diagnoses, because most children did not undergo follow-ups. Retrospectively, the diagnoses were assigned an OPH severity, ranging from high to low, as defined in Appendix 2 (https://doi.org/10.22470/pemj.2023.00843). Under this principle, specific diagnoses were classified by the OPH severity primarily based on relevant literature (1,11-13), and if remained uncertain, based on the opinion of a pediatric ophthalmologist (SA Chung). In cases where a child had multiple diagnoses, we chose a representative diagnosis, considering the severity and clinical context. Given the study objectives, diagnoses or procedures not requiring OPH referrals, such as an eyelid injury repair performed by an emergency physician, were not considered.
3. Statistical analysis
Data are presented as medians with interquartile ranges and as numbers and proportions for continuous and categorical variables, respectively. Variables were compared using Mann-Whitney U-tests, chi-square tests, chi-square tests for trend, or Fisher’s exact tests. Statistical significance was defined as P < 0.05. We used IBM SPSS Statistics for Windows, version 25.0 (IBM Corp) and MedCalc Statistical Software, version 18.6 (MedCalc Software bvba).
Results
1. Baseline characteristics of the study population
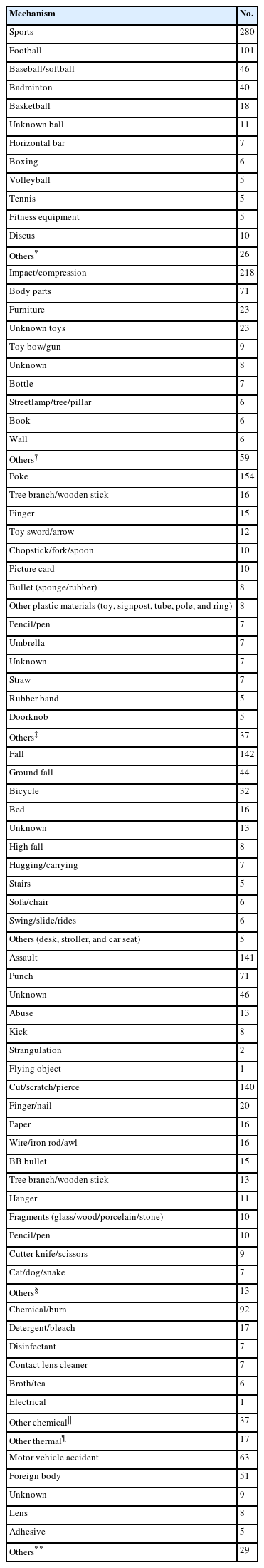
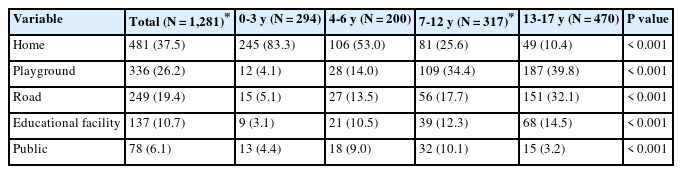
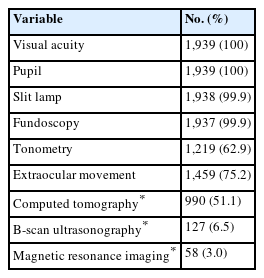
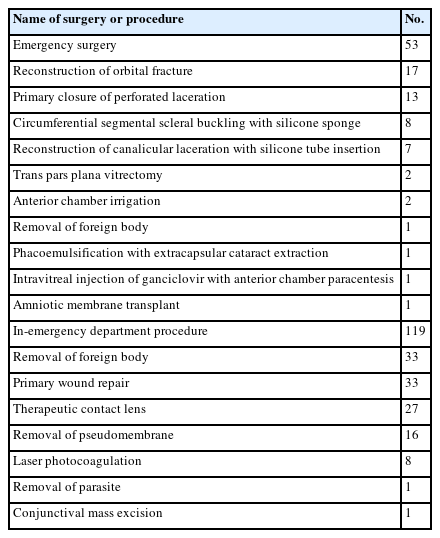
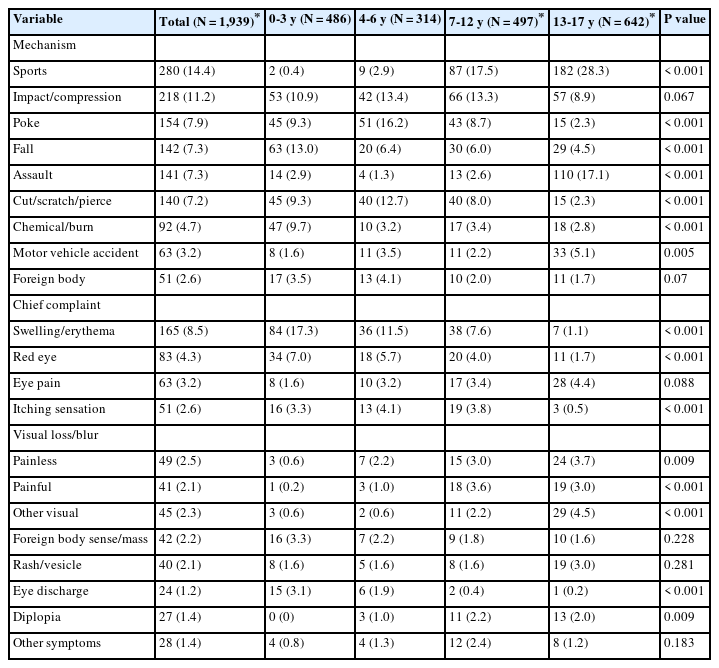
Of 1,978 eligible children, 1,939 were included in this study with a 66.1% proportion of injury (Fig. 1). The study population comprised 25.5% of the 7,595 children with eye-related symptoms who visited the ED during the study period. The median age of the population was 8.0 years (interquartile range, 3.0-14.0), and 623 children (32.1%) were girls. Visits at night, on weekend/holiday, and in fall accounted for 49.8%, 38.5%, and 32.1%, respectively. The most common injury mechanism and chief complaint were sports (14.4%) and swelling/erythema of the eye and adnexa (8.5%), respectively. The mechanisms are detailed in Appendix 3 (https://doi.org/10.22470/pemj.2023.00843). The most common place of injury was home (37.5%; Appendix 4, https://doi.org/10.22470/pemj.2023.00843). Most children underwent examinations for visual acuity, pupil, slit lamp, and fundoscopy, and 51.1% did computed tomography (Appendix 5, https://doi.org/10.22470/pemj.2023.00843). Emergency surgery, in-ED procedure, and hospitalization occurred in respectively 2.7%, 6.1%, and 2.5% (see details in Appendix 6, https://doi.org/10.22470/pemj.2023.00843).
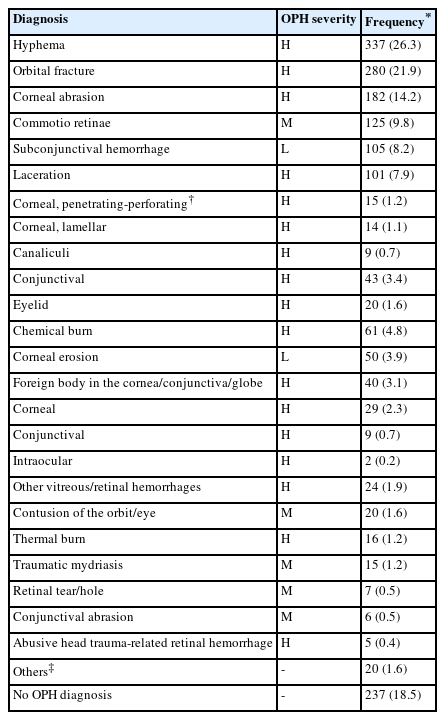
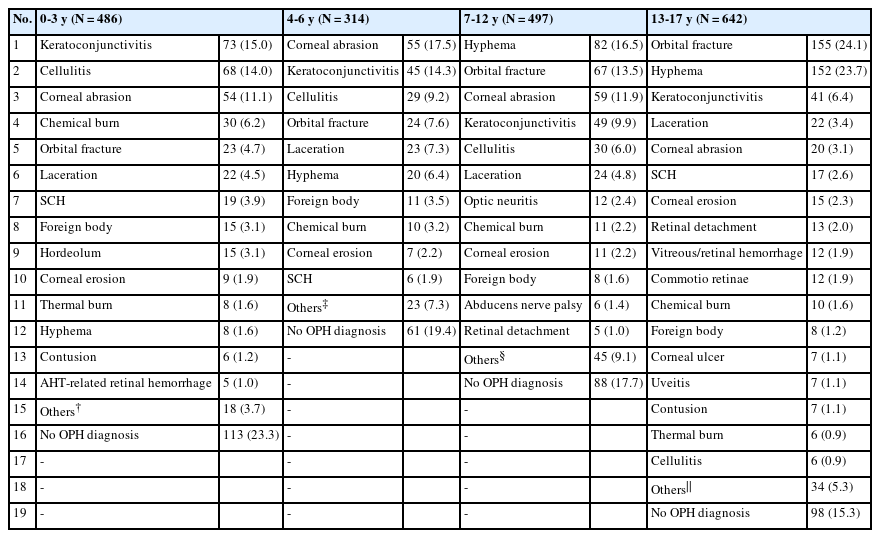
2. OPH diagnosis and severity
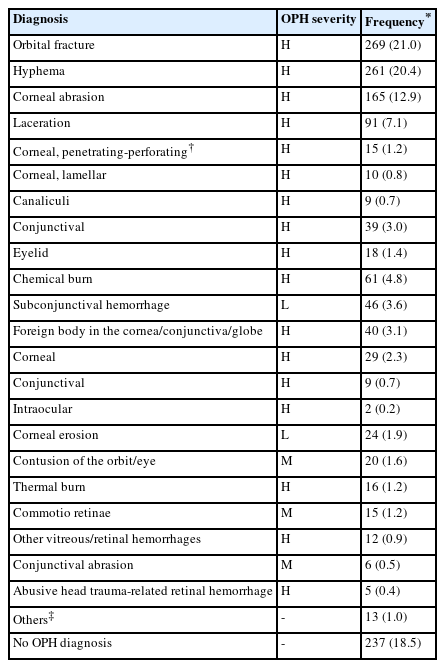
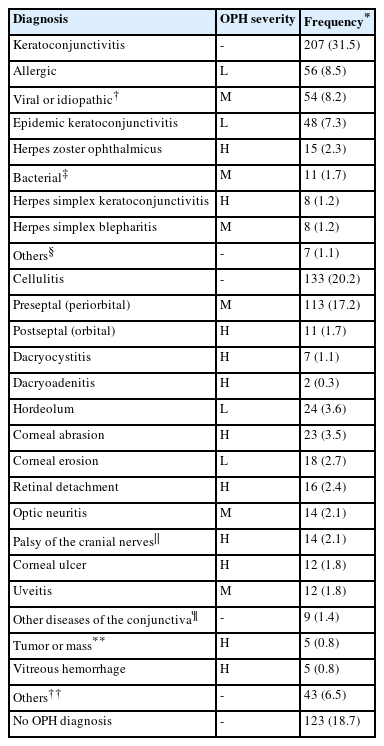
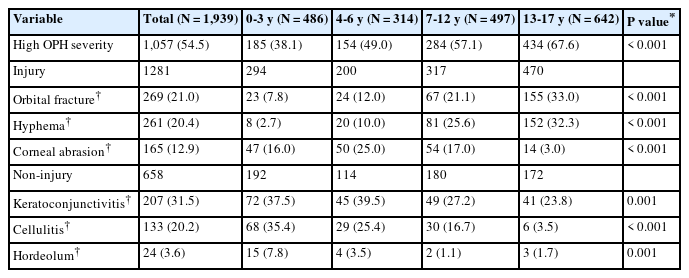
Tables 1 and 2 list the representative diagnoses related to injury and non-injury, respectively. Top 3 injuries were orbital fracture, hyphema, and corneal abrasion whereas top 3 non-injuries were keratoconjunctivitis, cellulitis, and hordeolum. In cases of injuries, we additionally listed all coexisting diagnoses given the frequent multiple injuries (Appendix 7, https://doi.org/10.22470/pemj.2023.00843).
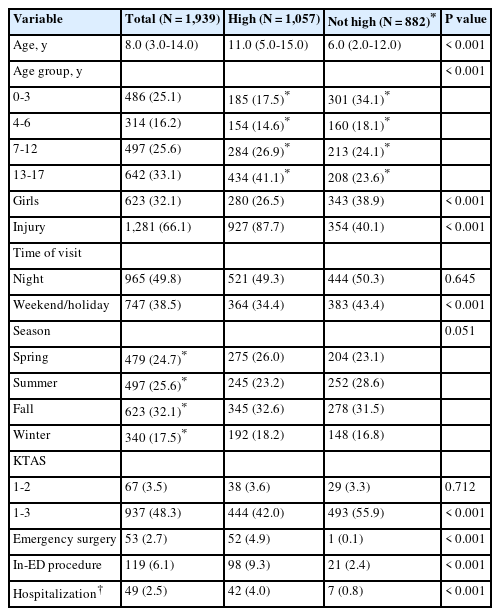
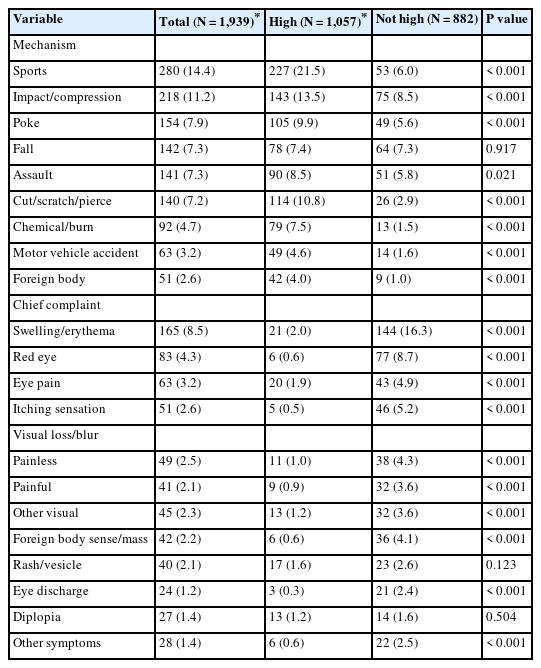
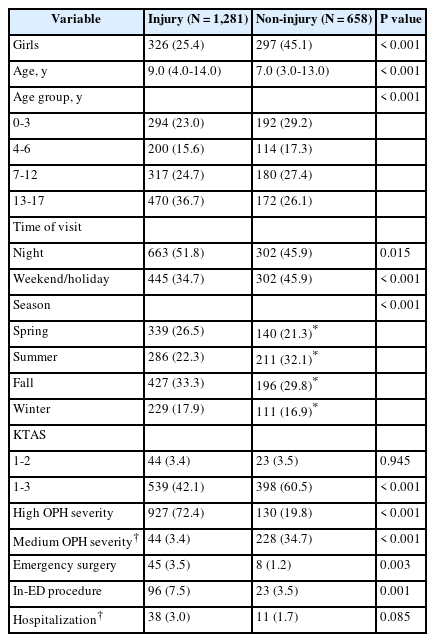
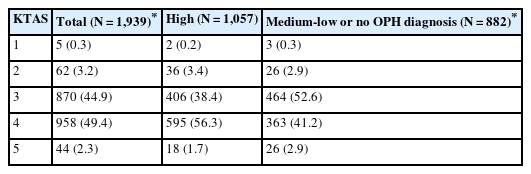
High OPH severity was associated with lower proportions of girls, visits on weekend/holiday, and most chief complaints, and with higher proportions of 13-17 years, injury, emergency surgery, in-ED procedure, hospitalization, and most injury mechanisms (Tables 3 and 4). There were 610 children (31.5%) with low OPH severity or no OPH diagnosis. No association was found between the high ED-assigned acuity (i.e., KTAS 1-2; 67 [3.5%]) and high OPH severity (1,057 [54.5%]) (Table 3). Most children (1,001 of 1,057 [94.7%]) with the high severity were assigned KTAS 3-4 (Appendix 8, https://doi.org/10.22470/pemj.2023.00843).
3. Comparisons of clinical features according to etiology and age groups
Table 5 shows that children with injury had a lower proportion of girls, visits on weekend/holiday, visits in summer, and a higher proportion of children aged 13-17 years, visits at night, visits in spring or fall, high OPH severity, emergency surgery, and in-ED procedure, compared to those with non-injury.
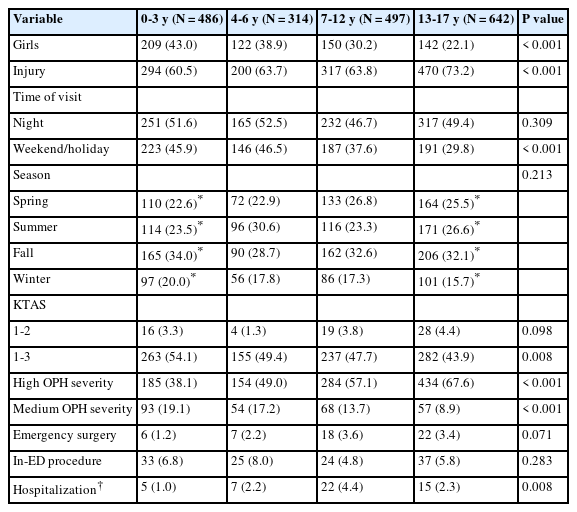
Table 6 shows a decrease in the proportion of girls and increases in injury and high OPH severity, with increasing age. Visits on weekend/holiday showed a decreasing trend with increasing age among children aged 4-17 years. Regarding the mechanism and chief complaint, sports, assault, eye pain, visual loss/blur, diplopia, and other visual symptoms tended to increase with age (Appendix 9, https://doi.org/10.22470/pemj.2023.00843). In contrast, the opposite trends were noted for poke, fall, cut/scratch/pierce, chemical/burn, swelling/erythema of the eye and its adnexa, red eye, itching sensation, and eye discharge. Older children tended to have injuries outside their homes (Appendix 4).
High OPH severity and the top 3 diagnoses are associated with the age groups (Fig. 2, Table 7, and Appendix 10 [https://doi.org/10.22470/pemj.2023.00843]). With increasing age, high OPH severity, orbital fracture, and hyphema increased in proportions whereas corneal abrasion, keratoconjunctivitis, cellulitis, and hordeolum tended to decrease (all Ps for trend ≤ 0.001).
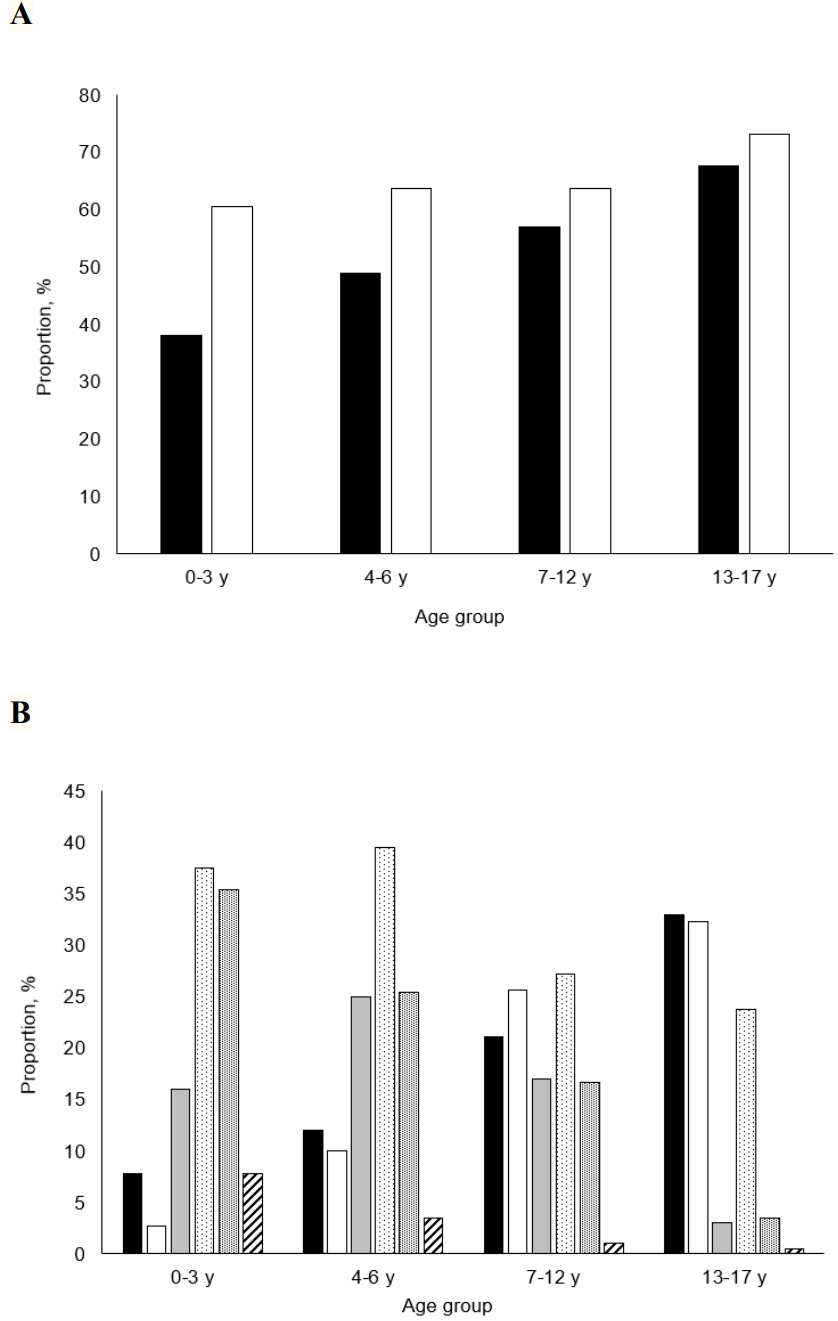
Comparison of high ophthalmic severity and injury and non-injury top 3 diagnoses according to age groups. (A) With increasing age, high severity (shaded bars) and injury (open bars) increase in proportions. (B) Orbital fracture (black shaded bars) and hyphema (open bars) increase with age. This trend contrasts with decreases in corneal abrasion (gray shaded bars), keratoconjunctivitis (stippled bars), cellulitis (fine stippled bars), and hordeolum (hatched bars) (see numerical data in Table 7).
Discussion
This study shows an association of high OPH severity with injury, older age, and boys. We discuss the dual implications for decision-making in children with eye-related symptoms who visit EDs. Children with high-to-medium severity probably have true OPH emergencies, which require emergency surgery, hospitalization, or expert opinion, compelling immediate referrals or transfers to ophthalmologists. Conversely, for children with low severity, emergency physicians or pediatricians may play some roles of on-call ophthalmologists in EDs, and divert the children to outpatient departments or outside clinics within a few days. The efficient use of emergency medicine resources is predicated on the non-ophthalmologists’ capability to make presumptive OPH diagnoses.
The study findings are consistent with those of a recent study performed in Wills Eye Hospital ED in terms of median age (9.8 years), the most common age group (15-18 years), injury mechanism (sports), and diagnosis (conjunctivitis) (8). As per a 2006-2014 United States Nationwide Emergency Department Sample (NEDS)-based study, “strike to the eye (22.5%)” was the most common mechanism, followed by “sports (14.2%),” which differs from the current study where sports were the predominant mechanism (13). This difference might stem from the higher proportion of injured children aged 10-17 years in our study (37.5% vs. 49.9% [639 of 1,281]) (13). Two Korean ED-based studies on ocular injury performed on patients of all ages listed “hyphema, eyelid laceration, and orbital fracture” and “corneal abrasion, orbital contusion, and hyphema” as the top 3 diagnoses, respectively (12,14). These diagnoses contain the top 3 injuries of the current study. Consistent with our study, the 2 Korean studies (12,13) reported football and baseball as the 2 most commonly causative sports activities (Appendix 3).
The association of injury with high OPH severity may be due to the following factors. First, trauma to the eye and its adnexa results in obvious wounds impacted by foreign bodies, or bleeding, which intuitively prompts emergency intervention. Second, OPH hospitalization is more frequent in injured children than in ill children (8). Third, by definition, an injury diagnosis is more likely to be regarded as highly severe than a non-injury diagnosis. As per a 2006-2011 United States NEDS-based study, a chief reference for the OPH severity, all diagnoses related to laceration or foreign bodies are categorized as “likely to be emergent (1).” In contrast, preseptal cellulitis, hordeolum, most conjunctivitis, and even optic neuritis are sorted as “nonemergent” or “could not be determined.” This categorization is in line with our rating of OPH severity (Tables 1 and 2).
The association of boys with high OPH severity may be related to the fact that 74.6% of the children with injuries are boys, which is inherently associated with the high severity of injuries (Table 5). Relevant studies show that boys account for 63%-68% of children with ocular injuries who visit EDs (13,15). The role of older age could be explained by the tendency for outside-the-home injuries in older children (Appendix 4) and age-related increases in sports, assault, eye pain, visual loss/blur, diplopia, and other visual symptoms (Appendix 9). For instance, if an adolescent with diplopia is diagnosed with benign oculomotor nerve palsy, he or she would be regarded as having a high OPH severity (1). The higher proportion of boys, older age, and higher OPH severity in our study are consistent with the findings of a Korean single ED-based study comparing children with general trauma and those with diseases (9).
In this study, 54.5%-68.5% of the children were considered candidates for OPH referrals. In EDs, in addition to high OPH severity, cases requiring only emergency OPH examinations (i.e., medium severity [14.0%]) can also be considered near emergencies. It is difficult to reduce such referrals. However, we found a minimal portion of potentially unnecessary referrals from children with low OPH severity or no OPH diagnosis (31.5%). The low-severity referrals can be decreased by enhancing emergency physicians’ or pediatricians’ knowledge and experience of OPH diseases and minor injuries. Depending on their clinical competence, the cutdown on unnecessary referrals may extend to some cases of medium OPH severity. The need for cutdown should be highlighted in infants or toddlers who require additional measures, such as procedural sedation and analgesia, for a detailed examination.
A discordance between KTAS 1-2 and OPH severity was observed, as exemplified by the fact that 3.6% of children with high severity were categorized as under KTAS 1-2 (Appendix 8). The discordance was also shown between KTAS 1-3 and the severity. This feature is likely due to the consideration of KTAS outside the primary diagnosis (e.g., vital signs) and the localized features of eye-related symptoms. Thus, emergency physicians or pediatricians may need to prioritize referrals or interventions for children with the symptoms, regardless of the initial KTAS.
Some miscellaneous findings are notable from the emergency medicine perspective. First, although most cases of conjunctivitis are classified as medium-to-low OPH severity, herpes simplex infection should be distinguished by the presence of vesicles or corneal dendrites owing to its potential for developing blindness and contraindications for frequently prescribed steroids. Second, we found 2 children with thelaziasis, infection by Thelazia callipaeda, of whom 1 underwent removal of the parasite (Appendix 6). This eye-specific parasite warrants attention in EDs, given its potential for causing keratitis and anxiety-provoking features in children or guardians. Third, because ball sports are commonly related to injuries, such as an orbital fracture or hyphema via ball-to-eye collision, protective eyewear should be used in a compulsory way (13,14).
This study has limitations. First, there might be inherent bias related to the single-center design. However, the study population is larger than that of the relevant Korean multicenter study (n = 446) (14). Second, given the lack of numerical data regarding visual acuity, we could not assess visual outcomes, irrespective of the diagnosis-based severity. Third, we could not determine the general conditions and diagnoses beyond the OPH scope because diagnoses made or procedures performed by ophthalmologists were the focus of data collection.
Briefly, true OPH emergencies may be more prevalent among injured, older, or male children. The study findings could help emergency physicians and pediatricians in directing their attention toward children exhibiting signs of true emergencies, thereby redirecting less urgent cases to outpatient departments or outside ophthalmology clinics.
Notes
Author contributions
Conceptualization, Data curation, Resources, and Software: Y Cha and JH Kim
Formal analysis, Investigation, and Methodology: all authors
Project administration and Validation: JH Kim and SA Chung
Supervision and Visualization: JH Kim
Writing-original draft: Y Cha and JH Kim
Writing-review and editing: all authors
All authors read and approved the final manuscript.
Conflicts of interest
JH Kim has served as an editor of Pediatric Emergency Medicine Journal since 2014, and was not involved in the review of this paper. Otherwise, no potential conflicts of interest relevant to this article were reported.
Funding sources
No funding source relevant to this article was reported.