Impact of non-pharmaceutical interventions on the rate of respiratory viruses other than severe acute respiratory syndrome coronavirus 2 in the coronavirus disease 2019 pandemic
Article information
Abstract
Purpose
We aimed to evaluate the impact of non-pharmaceutical interventions (NPIs) on the transmission of respiratory viruses other than severe acute respiratory syndrome coronavirus 2 among children during the coronavirus disease 2019 pandemic.
Methods
We analyzed the clinical and polymerase chain reaction (PCR) findings using electronic medical records of children (< 18 years) with fever or respiratory symptoms who were hospitalized via the emergency department of Wonkwang University Hospital (Iksan, Korea), from March 2018 through December 2021. The children were divided into before and after groups based on the hospitalization date relative to February 2020, starting point of the implementation of NPIs. PCR was performed using nasopharyngeal swab samples. Between the 2 groups, we compared age, sex, length of hospital stay, and PCR findings.
Results
The before and after groups consisted of 3,160 and 989, respectively, showing a 68.7% decrease in the number of children undergoing PCRs after the implantation of NPIs. The after group showed higher median values of the age and length of hospital stay than the before group (Ps < 0.001). A 76.9% decrease was noted in the number of children having PCR positivities (from 1,101 [34.8%] to 254 [25.7%]; P < 0.001). Among detected viruses, an increase in the proportion was noted only in human bocavirus (from 81 [2.6%] to 54 [5.5%]; P < 0.001). In contrast, significant decreases in the proportions were found in adenovirus, enterovirus, influenza A and B, respiratory syncytial viruses A and B, human coronaviruses (229E, NL63, and OC43) and human metapneumovirus.
Conclusion
NPIs may be effective in reducing the transmission of respiratory viruses other than severe acute respiratory syndrome coronavirus 2 among children during the pandemic.
Introduction
Owing to the coronavirus disease 2019 pandemic, many countries have implemented measures to prevent the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)1). Non-pharmaceutical interventions (NPIs) are a set of measures other than vaccinations or drugs that helps slow the spread of infections, including wearing of face masks, social distancing, intensive contact tracing and isolation, and disinfection2) (Appendix 13) , https://doi.org/10.22470/pemj.2023.00710). Since February 2020, the Korean government has been implementing the NPIs. The strict enforcement of NPIs has also affected the spread of other viruses with transmission routes similar to that of SARS-CoV-22) . Unlike adults, children have relatively low incidences of chronic and metabolic diseases and higher rates of viral infection-related hospital visits. Hence, we aimed to investigate the effectiveness of the NPIs on each respiratory virus other than SARS-CoV-2 during the pandemic using microbiological findings in hospitalized children.
Methods
We analyzed the clinical and polymerase chain reaction (PCR) findings using electronic medical records of children (< 18 years) with fever or respiratory symptoms who were hospitalized in the pediatric department, via the emergency department of Wonkwang University Hospital (Iksan, Korea), from March 2018 through December 2021. The hospital is the only tertiary hospital in western Jeollabuk-do and southern Chungcheongnam-do. The exclusion criteria are listed in Fig. 1. This study was approved by the institutional review board of the Hospital (IRB no. 2022-12-024). Informed consent was waived because the study only used aggregate epidemiological data without patient or clinician identifiers.
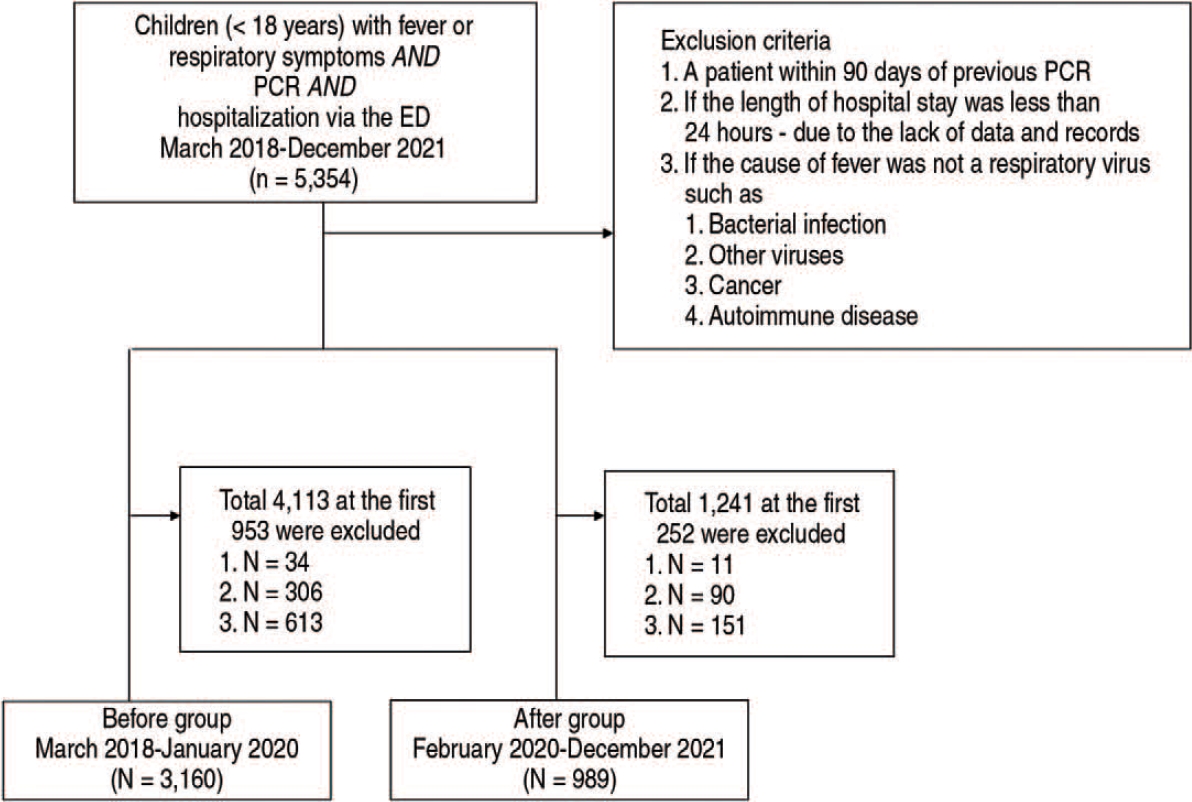
Flowchart for the selection of the study population. PCR: polymerase chain reaction, ED: emergency department.
The clinical findings included age at hospital visit (month), sex, and length of hospital stay (day). Nasopharyngeal swab samples were analyzed using PCR kits, Allplex Respiratory Panel 1-3 (Seegene, Seoul, Korea), and CFX96 real-time system (BioRad, Hercules, CA), which can detect adenovirus, human coronaviruses (229E, NL63, and OC43), influenza A and B, human bocavirus, enterovirus, rhinovirus, human metapneumovirus, parainfluenza, and respiratory syncytial viruses (RSV) A and B. If 2 or more viruses were detected in a child, the child was regarded to have a coinfection. The study population was dichotomized into before and after groups based on the hospitalization date relative to February 2020, the starting point of implementation of the NPI.
We used chi-square test and Mann-Whitney U-tests to identify the differences between the before and after groups. Statistical significance was defined as P < 0.05. All statistical analyses were performed using IBM SPSS ver. 25.0 (IBM Corp., Armonk, NY).
Results
Of 5,354 eligible children, we analyzed 4,149 children, among whom 3,160 belonged to the before and 989 to the after group (Fig. 1). This shows 68.7% decrease after the implantation of NPIs in the numbers of children with fever or respiratory symptoms who underwent PCRs.
The comparison of clinical and PCR findings between the 2 groups is summarized in Table 1. Median values of the children’s age and length of hospital stay were higher in the after group. A 76.9% decrease was noted in the number of children having PCR positivity. In the order of proportion (highest to lowest), we noted rhinovirus, adenovirus, and parainfluenza in the before group, and rhinovirus, human bocavirus, and parainfluenza in the after group. The number of detected viruses decreased overall, and only human bocavirus increased in the proportion. All other viruses but rhinovirus and parainfluenza decreased in their proportion. The after group showed sharp decreases in the number of detected viruses and their peaks after February 2020, the first month of implementation of the NPIs (Fig. 2).

Comparison of clinical and PCR findings between before and after the implementation of non-pharmaceutical interventions (n = 4,149)

Monthly trends of PCR findings before (A) and after (B) the implementation of non-pharmaceutical interventions. The before group showed 4 peaks: May 2018, December 2018, April 2019, and December 2019 (A). In contrast, the after group showed a sharp decrease in the number of detected viruses with only 1 peak (October 2021). PCR: polymerase chain reaction.
Discussion
This study shows a potential impact of the NPIs on the transmission of respiratory viruses other than SARS-CoV-2 in children with fever or respiratory symptoms who underwent PCR and hospitalization via the emergency department. In particular, a 76.9% decrease was noted in the number of children having PCR positivity. Among detected viruses, most decreased in their numbers and proportions, except human bocavirus which increased in its proportion. Despite the single center study setting, the findings may represent the overall picture in the region because the center is the only tertiary hospital in western Jeollabuk-do and southern Chungcheongnam-do, which primarily treated children with potential infection during the pandemic. Unlike other studies, most children having signs of infection were included and underwent PCRs, resulting in accurate findings.
We speculated the reasons why the potential impact of the NPIs was different among the viruses. This difference cannot be explained by the transmission routes since the routes of all viruses in this study were similar4-6). The after group showed less prominent seasonal peaks than the before group (Fig. 2). Hence, a seasonal virus might have spread less avidly due to the implementation of NPIs. This speculation is consistent with the decreases in influenza and RSV, which cause high fever or respiratory distress in specific seasons. In contrast, the relatively less affected virus was rhinovirus, which causes infection throughout the year.
A narrative review authored by Karimzadeh et al.7) compared infectious doses of human coronavirus, influenza, rhinovirus, adenovirus, coxsackievirus, and RSV, showing that the infectious dose of rhinovirus was the lowest. This finding coincides with the unaffected proportion of rhinovirus in the midst of overall decrease in most other viruses in our study. The review did not discuss human bocavirus whose proportion increased in our study. Therefore, viruses with low infectious doses were transmitted at a relatively high rate, even in a situation where propagation was mitigated by the implementation of the NPIs.
Viruses of smaller sizes are associated with a higher incidence of outbreaks8). Rhinovirus and human bocavirus measure about 30 nm and 20 nm in diameter, respectively9). This association can be attested by the unreduced rate of rhinovirus and human bocavirus in our study. However, with the exception of the 2 viruses, no association was found between the size and change in proportion.
This study has several limitations of note. First, no causation could be known between the NPIs and PCR findings. In addition to evaluating the infectious doses, more investigations are needed on the transmission and infection rates according to specific viruses. Second, an association was not observed between changes in the NPIs and PCR findings. Although implementation of the NPIs was described, we did not keep track of continuous changes in the details, such as the number of people allowed in a gathering or whether official events can be held. It is necessary to address this issue in the future.
In conclusion, NPIs may be effective in preventing the transmission of respiratory viruses other than SARS-CoV-2 among children during the coronavirus disease 2019 pandemic.
Notes
Conflicts of interest
No potential conflicts of interest relevant to this article were reported.
Funding sources
No funding source relevant to this article was reported.

