빠르게 진행하는 수두증을 동반한 리스테리아 수막염: 열성 뇌전증지속상태를 첫 증상으로 보인 16개월 여아 1례
Listeria meningitis with rapid progression of hydrocephalus: a case of a 16-month-old girl with febrile status epilepticus as the first symptom
Article information
Trans Abstract
Listeria monocytogenes is a rare cause of bacterial meningitis, particularly beyond the neonatal period. This article describes a 16-month-old girl who presented with a new-onset febrile status epilepticus, and subsequently developed altered mentality and lethargy. L. monocytogenes was detected on a point-of-care, multiplex polymerase chain reaction using the cerebrospinal fluid. On day 3, she developed a rapidly progressive hydrocephalus. Her consciousness improved after placement of an external ventricular drain. After 3-week antibiotic therapy, she was successfully discharged without residual complications.
Introduction
Listeria monocytogenes is a facultatively anaerobic, non-spore-forming, motile, gram-positive bacillus that typically affects pregnant women, newborns, immunocompromised individuals, and older adults1). The common route of transmission is the gastrointestinal tract. Except in neonates, Listeria infections usually present as acute gastroenteritis, but rarely do as meningitis. Listeria meningitis differs from other bacterial meningitis in the regimen of empirical antibiotics. Although it is rare in immunocompetent children, hydrocephalus can rapidly complicate the outcome. It is critical to diagnose and treat the disease entity in a timely manner2). Here, we report a toddler with Listeria meningitis with rapidly progressive hydrocephalus that started with febrile status epilepticus (FSE). This study was approved by the institutional review board of Kangdong Sacred Heart Hospital with a waiver for informed consent (IRB no.2022-09-023).
Case
A previously healthy, fully vaccinated 16-month-old girl visited another emergency department (ED) with 1-day history of fever and a new-onset FSE lasting 25 minutes (5 days before the visit to us). After the arrival, the generalized seizure stopped spontaneously. She was discharged without further evaluation because she became alert. Subsequently, she had poor oral intake and decreased activity. Three days before the visit to us, vomiting and diarrhea had been started. She visited our ED with lethargy 5 days after the FSE.
The initial vital signs were as follows: blood pressure, 100/60 mmHg; heart rate, 150 beats/minute; respiratory rate, 20 breaths/minute; temperature, 39.2°C; oxygen saturation, 99% on room air; and a Glasgow Coma Scale of 12, with normal pupil light and deep tendon reflexes. Physical examination showed no other signs, such as focal weakness, setting sun sign, respiratory distress or skin lesions. The girl did not eat contaminated foods or make contact domestic animals. Initial laboratory findings were as follows: white blood cells, 8.5 × 103/µL with 71% neutrophils; hemoglobin, 11.6 g/dL; erythrocyte sedimentation rate, 32 mm/hour; C-reactive protein, 133.5 mg/L; glucose, 206 mg/dL; serum natrium, 127 mEq/L; and urine natrium, 8 mEq/L. After 0.9% saline hydration for 2 hours, the serum natrium concentration was 129 mEq/L, but she remained stuporous. Brain computed tomography (CT) scan showed asymmetry of the left lateral ventricle without a remarkable hydrocephalus (Fig. 1A).
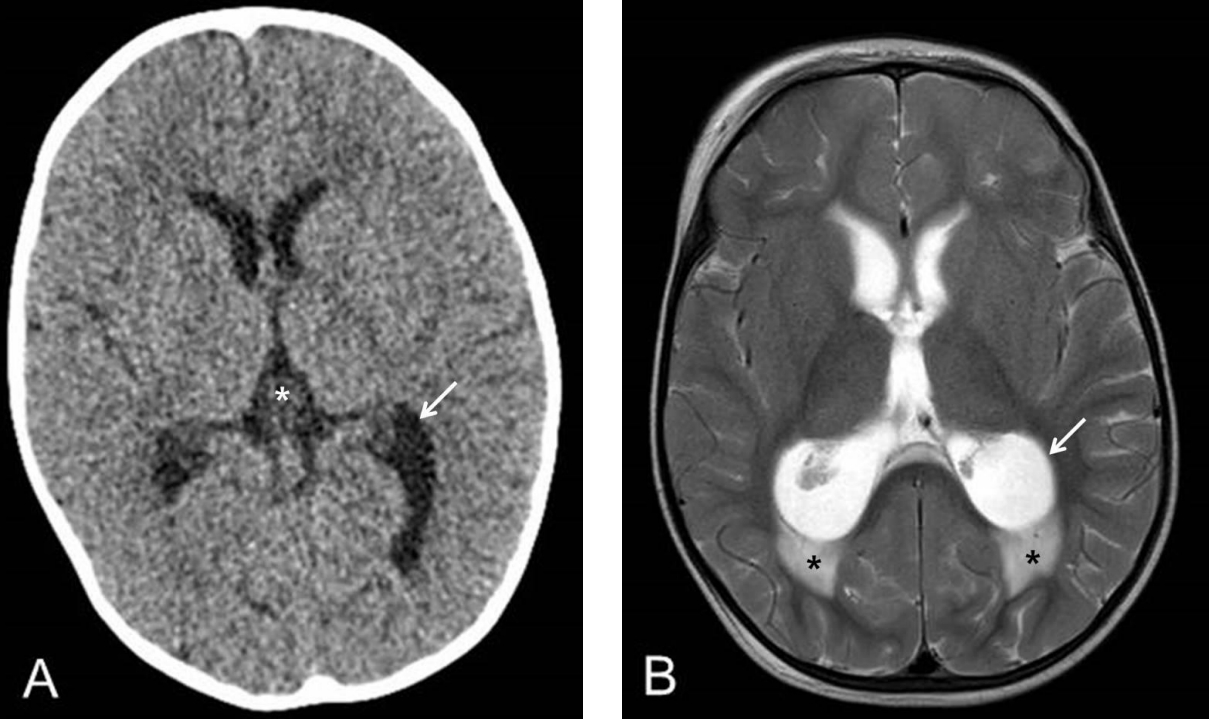
Rapid progression of hydrocephalus due to Listeria meningitis. Computed tomography scan on day 1 shows asymmetry of the occipital horn of the left lateral ventricle (arrow, A) and dilated third ventricle (asterisk, A). T2 fluid-attenuated inversion recovery magnetic resonance imaging on day 3 shows both lateral and third ventricles enlarged, particularly the occipital horns (arrow, B). There is also diffuse periventricular edema just posterior to the horns (asterisks, B).
On day 2, the girl continued to have intermittent spikes in fever and diarrhea. Given the persistent stupor and fever, lumbar puncture (LP) was performed. Cerebrospinal fluid (CSF) profile suggested bacterial meningitis as follows: white blood cells, 146/mm3 with 85% neutrophils; red blood cells, 80/mm3; glucose, 3 mg/dL; and protein, 266 mg/dL. She received intravenous ampicillin-sulbactam (ampicillin, 300 mg/kg/day), cefotaxime (300 mg/kg/day), and vancomycin (60 mg/kg/day). She had difficulty sitting up on her own, and was irritable all day. L. monocytogenes was positive on a point-of-care, multiplex polymerase chain reaction (PCR) (RFIT-ASY-0119, RFIT-ASY-0118; BioFire Diagnostics, Salt Lake City, UT) using the CSF. Subsequently, amikacin (20 mg/kg/day) was added to, and cefotaxime was removed from the empirical antibiotics. The PCR finding was confirmed by CSF culture. Immunoglobulin concentrations were within the normal ranges for her age.
On day 3, her fever decreased, but due to worsening mental status (Glasgow Coma Scale, 11), we performed magnetic resonance imaging (MRI) 42 hours after the CT (Fig. 1B). The MRI showed rapidly progressing communicating hydrocephalus with diffuse periventricular edema. Given the unavailability of emergency decompression of the hydrocephalus in our hospital, she was transferred to a tertiary hospital on the same day.
On the day after the transfer, an external ventricular drain was inserted. Antibiotics were changed to ampicillin (300 mg/kg/day) and gentamicin (5 mg/kg/day) with no growth on follow-up cultures of the CSF and blood. After the insertion, she became able to move per the physicians’ directions. On postoperative day 12, the drain was removed. On postoperative day 19, a follow-up CT showed the improved hydrocephalus. After 3-week antibiotics therapy, she was discharged from the tertiary hospital, without a residual complication (23 days after the visit to our hospital).
Discussion
At EDs, children with new-onset febrile seizure aged 12-18 months need clinical assessment, observation, and selective LP for timely diagnosis of bacterial meningitis. CSF profile is needed to differentiate meningitis if a seizure lasts longer than 30 minutes, or is followed by prolonged postictal state or focal neurologic deficits3). In the present case, we performed LP 6 days after the FSE, recognizing the persistent stupor after the FSE. This indicates the importance of 2- or 5-day observation for children hospitalized with FSE.
In cases of bacterial meningitis suspected on initial CSF profiles, commonly used empirical antibiotics for children older than 2-3 months do not cover L. monocytogenes due to its rarity. For the bacterium, ampicillin and aminoglycoside are preferred4). Administration of beta-lactam antibiotics may reduce the odds of 3-month mortality of Listeria bacteremia or meningitis to 0.15). The aforementioned multiplex PCR can detect 14 pathogens, e.g., Escherichia coli and L. monocytogenes, in CSF samples within a few hours. In our case, despite the delayed timing of LP, it was possible to detect L. monocytogenes with the PCR and adjust antibiotic regimen in time6).
Listeria meningitis infection initially presents with atypical symptoms, such as fever, diarrhea, headaches, nausea, vomiting, and myalgia. However, it may cause hydrocephalus, cerebritis, ventriculitis, and brain abscess5). The case patient developed rapid progressive communicating hydrocephalus on the MRI performed 42 hours after the initial CT. Serial neuroimaging is helpful in determining the insertion of external ventricular drain or other measures to reduce intracranial pressure if the consciousness worsens, even after the antibiotic therapy.
In conclusion, our case shows that Listeria meningitis should be considered in immunocompetent children even with the new-onset febrile seizure, and that novel multiplex PCR allows rapid detection of bacterial pathogens, such as L. monocytogenes.
Notes
Conflicts of interest
No potential conflicts of interest relevant to this article were reported.
Funding sources
This research was supported by the Hallym University Kangdong Sacred Heart Hospital Research Fund (grant no. 2021-04).
