가슴불편감으로 응급실을 방문한 청소년의 임상적 특성: 기저질환 인식의 중요성
Clinical features of adolescents who visited the emergency department with chest discomfort: the importance of recognizing underlying medical conditions
Article information
Trans Abstract
Purpose
We aimed to evaluate the clinical features of adolescents who visit emergency departments (EDs) with chest discomfort, and analyze the implications of underlying medical conditions for the development of cardiogenic chest discomfort.
Methods
We reviewed the medical records of adolescents (13-18 years) with chest discomfort who visited a tertiary hospital ED in Seoul, Korea from 2014 through 2018. Sex, age, duration and character of the discomfort, symptoms and signs, ED length of stay, abnormal findings of vital signs, chest radiograph, electrocardiogram, and elevated concentrations of cardiac enzymes were reviewed. Final diagnosis was based on cardiac evaluations within 1 year after the index visit. Underlying medical conditions were defined as visits to the cardiology, pulmonology or hematology-oncology clinics at least twice in the preceding year. Initial suspicious clinical findings were defined as palpitation, syncope or high blood pressure. Logistic regression was used to identify predictors for cardiac etiology.
Results
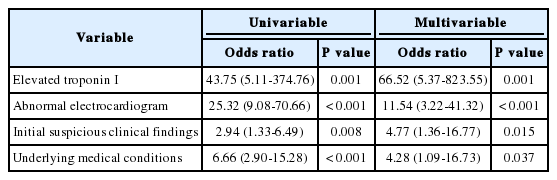
Of the 231 patients, 43 (18.6%) and 69 (29.9%) had underlying medical conditions and initial suspicious clinical findings, respectively. The predictors for cardiac etiology were underlying medical conditions (odds ratio, 4.28; 95% confidence interval, 1.09-16.73), initial suspicious clinical findings (4.77; 1.36-16.77), abnormal electrocardiogram (11.54; 3.22-41.32), and elevated concentration of troponin I (66.52; 5.37-823.55). The patients with cardiogenic chest discomfort had a longer median ED length of stay (281.0 minutes [interquartile range, 215.5-369.0] vs. 199.5 [132.8-298.0]; P = 0.004) and a higher hospitalization rate (48.3% vs. 13.4%; P < 0.001) than those with non-cardiogenic chest discomfort.
Conclusion
It may be necessary to recognize underlying medical conditions and initial suspicious clinical findings in EDs prior to cardiac evaluation in adolescents with chest discomfort.
Introduction
Approximately 0.3%-0.6% of pediatric patients who visit emergency departments (EDs) present with chest discomfort, and 16% of them make return visits[1-5]. In addition, 13% of pediatric patients who visit EDs have chest pain as an associated symptom[6]. The etiology of pediatric chest discomfort varies, and is frequently non-cardiac[1,7-10]. Only 0.5%-5% of pediatric patients with chest discomfort have cardiogenic causes, such as arrhythmia, pericarditis, and myocarditis[3,8,11,12]. Consistent with this, a previous Korean study on pediatric patients who visited an ED with chest discomfort reported that cardiogenic and idiopathic chest discomforts accounted for 3.8% and 73.6%, respectively[9].
Despite the low rate of cardiogenic chest discomfort in pediatric patients, caregivers’ concerns are serious, resulting in a 5%-39.3% rate of consultation with cardiologists[4,8,10,12]. Accordingly, recent studies have raised concerns on unnecessary consultations and cardiac evaluations related to chest discomfort[1,4,8,12]. However, we found a lack of data on the predictors for cardiogenic chest discomfort among adolescents, especially in those with underlying medical conditions. Hence, we aimed to investigate the rates of diverse etiology of chest discomfort in adolescents in the ED, and more importantly, predictors for cardiac etiology in the adolescents.
Methods
1. Study design and setting
Patients aged 13-18 years who visited the ED from 2014 through 2018 with chest discomfort as the chief complaint were included in this study. Patients who were transferred to other institutions were excluded. The patients with chest discomfort underwent routine measurements of initial vital signs, history taking, and physical examination. Cardiac evaluations were performed at each physician’s discretion. This study was approved by the institutional review board of Samsung Medical Center, which waived the requirement of obtaining informed consent due to the retrospective design (IRB no. 2020-03-071).
2. Definitions of terms
Underlying medical conditions were operationally defined as visits to cardiology, pulmonology or hematology-oncology clinics at least twice in the preceding year. Data were collected regarding the diagnoses that formed the reason for visiting the outpatient clinics. Initial suspicious clinical findings were defined as initial palpitation, syncope or high blood pressure because these signs are related to cardiac etiology. Any findings of chest radiographs other than the report of “no active lung lesions” by radiologists and electrocardiographic (ECG) findings other than sinus rhythm with common variations were considered abnormal. Elevated cardiac enzymes were defined as concentrations greater than the 99% cutoff for troponin I (TnI, > 0.04 ng/mL) and for creatine kinase-MB fraction (CK-MB, > 5.0 ng/mL) or a 4-fold increase in follow-up tests[13]. The final diagnosis was established based on cardiac evaluations performed within 1 year after the ED visit. By this diagnosis, the adolescents were divided into the cardiogenic and non-cardiogenic groups.
3. Data collection
We retrospectively reviewed the medical records of the ED visits, hospitalization, and the above-mentioned clinics from the preceding year of the ED visits to 1-year follow-up. Variables obtained were sex, age, duration (day) and character (e.g., squeezing) of chest discomfort, associated symptoms and signs, ED length of stay (minute), underlying medical conditions, initial suspicious clinical findings, abnormal findings of vital signs, chest radiograph, ECG, and elevated cardiac enzymes.
4. Statistical analysis
A chi-square tests and Mann-Whitney U tests were used to evaluate differences in categorical and continuous variables, respectively. Covariates with P < 0.1 on univariable analysis were entered into a multivariable logistic regression model. Multicollinearity between independent variables was assessed by the variance inflation factor (VIF) values, and any variable with a VIF higher than 4 was excluded. A P < 0.05 was considered significant. We used IBM SPSS Statics for Window ver. 25.0 (IBM Corp., Armonk, NY).
Results
1. Clinical characteristics of the patients
From 2014 through 2018, 240 adolescents with chest discomfort visited the ED, of whom, 9 were excluded from the study by the exclusion criterion. The characteristics of the study population are summarized in Table 1. Most patients experienced chest discomfort for less than a day (64.1%), and complained of experiencing the squeezing type of chest discomfort (35.5%). Forty-three patients (18.6%) had underlying medical conditions (see details of the diagnoses in Appendix 1, https://doi.org/10.22470/pemj.2020.00101). Sixty-nine (29.9%) patients presented with initial suspicious clinical findings. Cardiac murmurs or irregular heartbeats were noted in 4.3% of patients. The median ED length of stay was 209 minutes (interquartile range, 133.3-300.0) with a longer median length in the cardiogenic group than in the non-cardiogenic group (281.0 vs. 199.5 minutes; P = 0.004). Hospitalization rate was 17.7% (41 patients) with a higher rate in the cardiogenic group (48.3% vs. 13.4%; P < 0.001). Two patients were hospitalized in the intensive care unit. The sole mortality occurred in a 13-year-old boy with acute myocarditis superimposed on underlying dilated cardiomyopathy. Although he underwent extracorporeal membrane oxygenation for several months while awaiting a heart transplant, the cause of mortality was presumed to be intracranial hemorrhage.
2. Etiology of chest discomfort
Idiopathic origin was most common (45.0%), followed by pulmonary, cardiovascular, gastrointestinal, musculoskeletal, and psychiatric diseases (Fig. 1). In the cardiogenic group, arrhythmia was the most common diagnosis, followed by pulmonary hypertension, cardiomyopathy, myocarditis or pericarditis, vascular disease, vasovagal syncope, and cardiac rhabdomyosarcoma.

Etiology of chest discomfort (n = 231). Idiopathic origin was most commonly reported (n = 104 [45.0%]). Others were pulmonary (n = 42 [18.2%]), cardiovascular (n = 29 [12.6%]), gastrointestinal (n = 25 [10.8%]), musculoskeletal (n = 16 [6.9%]), and psychiatric diseases (n = 10 [4.3%]). The cardiovascular diseases included arrhythmia (n = 10 [34.5%]), pulmonary hypertension (n = 6 [20.7%]), cardiomyopathy (n = 4 [13.8%]), myocarditis or pericarditis (n = 3 [10.3%]), vascular diseases (n = 3 [10.3%]), vasovagal syncope (n = 2 [6.9%]), and cardiac rhabdomyosarcoma (n = 1 [3.4%]).
3. Comparison between the cardiogenic and the non-cardiogenic groups
No differences in sex, age, and duration of symptoms were found between the 2 groups. However, there were more patients with initial suspicious clinical findings and elevated cardiac enzymes in the cardiogenic group than in the non-cardiogenic group. Abnormal ECGs were also reported more often in the cardiogenic group (Table 2).
4. Independent predictors for development of cardiogenic chest discomfort
Elevated TnI, abnormal ECGs, initial suspicious clinical findings, and underlying medical conditions were entered into a multivariable logistic regression model. The presence of underlying medical conditions was independently associated with the development of cardiogenic chest discomfort (odds ratio, 4.28; 95% confidence interval, 1.09-16.73). The other independent predictors are listed in Table 3. Although CK-MB was entered into the model, the variable was excluded from the final analysis given its VIF higher than 4.
Discussion
This study shows that the adolescents with underlying medical conditions were approximately 4.3 times more likely to develop cardiogenic chest discomfort than those without the conditions. In addition, the presence of initial suspicious clinical findings was associated with an approximately 4.8-fold increase in developing the symptom.
Previous studies have shown that an idiopathic chest discomfort is the most common diagnosis among the pediatric population with a 0.5%-5% rate of cardiac etiology[3,8,11,12]. Although idiopathic origin was also most common in our study, we noted a higher rate of cardiac etiology and lower rates of musculoskeletal and psychiatric origins, compared to the equivalent values in the previous studies[1,5,8,9,14]. This difference in etiology might stem from a higher proportion of patients with underlying medical conditions in this present study. None of the 43 patients with underlying medical conditions had an acute illness. Most previous studies were based on the general population or excluded patients with underlying medical conditions[6,8,12,14,15].
The initial suspicious clinical finding is a potential predictor for cardiogenic chest discomfort. This operational definition was based on the most diligently recorded symptoms, such as syncope. Massin et al.[1] reported dyspnea and palpitation as significant findings for cardiogenic chest discomfort at the ED. Other studies have also reviewed various manifestations, such as palpitation, dyspnea, syncope, and dizziness, in pediatric patients and adults aged up to 22 years with chest discomfort[8,10,12]. However, there is a lack of data on the role of the symptoms as predictors for cardiac etiology. Additionally, there is little data on whether high blood pressure is a predictor for cardiac etiology in adolescents. However, a previous study has shown that left ventricular hypertrophy and vascular remodeling seen with hypertension could also increase the cardiovascular risk in pediatric patients[16].
Assays for cardiac enzymes are traditionally used in EDs as simple methods to seek cardiac etiology. Although concentration of TnI was not measured in some patients in this study (Table 2), elevated TnI was more frequently observed in the cardiogenic group (25.9% vs. 0.8%). Conversely, several studies have reported no differences in TnI concentration between pediatric patients with and without cardiogenic chest discomfort[15,17-20]. However, these findings should be cautiously interpreted because elevated TnI is also found in chest trauma, sepsis, intoxication or substance abuse[21].
Abnormal findings of ECG should be interpreted carefully with consideration of other explanations. ECG is easily obtained and repeated at EDs[22]. In the present study, abnormal ECGs were more frequently found in the cardiogenic group, which is consistent with a previous report[14]. However, abnormal ECGs also occur in other conditions, such as poisoning due to caffeine or energy drinks[18-20,23]. The abnormal ECGs can be seen after correction of cardiac anomalies without clinical implications, such as right bundle branch block after correction of ventricular septal defect[24].
Given the single-center and retrospective design, this study has several limitations. First, patients were not systemically evaluated and followed up. This flaw caused missing data, especially the description of symptoms and signs. Second, underlying medical conditions were operationally defined as a history of visits to the specific clinics given the medical environment of tertiary hospitals. This coarse definition may be less generalizable to other settings. However, the use of the definition helped to screen patients with significant underlying medical conditions.
In conclusion, in addition to elevated concentration of TnI and abnormal ECGs, the underlying medical conditions and initial suspicious clinical findings may be associated with the development of cardiogenic chest discomfort in adolescents with chest discomfort.
Notes
Conflicts of interest
No potential conflicts of interest relevant to this article were reported.
Acknowledgements
No funding source relevant to this article was reported.