 |
 |
AbstractPurposeDuring the coronavirus disease 2019 pandemic, many countries have reported sharp drops in the numbers of patients, especially children, seeking emergency care unrelated to the disease. The author investigated the patterns of febrile children’s visits to the emergency department (ED) of a tertiary hospital from 2017 through 2020.
MethodsWe compared the data of febrile children aged 15 years or younger who visited the ED in 2017-2019 and in 2020 (February through August, each year). Information on the children’s baseline characteristics, the Korean Triage and Acuity Scale 1-2 indicating a high severity, and ED disposition, such as hospitalization, were collected. In addition, we determined the number of children who underwent cancellation, defined as the leave of children without treatment, and the rates of respiratory virus polymerase chain reaction performance and its positivity.
ResultsIn 2020, we noted decreases in the median monthly fever-related ED visits (2017-2019, 326 [interquartile range, 292-425] vs. 2020, 149 [132-182]; P < 0.001) with a shorter median fever duration (2017-2019, 11 [3-27] days vs. 2020, 9 [2-23] days; P < 0.001). However, in the same year, we noted increases in rates of the Korean Triage and Acuity Scale 1-2 (2017-2019, 5.7% vs. 2020, 16.4%; P < 0.001) and hospitalization (2017-2019, 23.5% vs. 2020, 35.7%; P < 0.001). We also noted increases in the number of cancellation and the rate of respiratory virus polymerase chain reaction performance rate, along with a decrease in its positive rate in 2020.
IntroductionThe coronavirus disease 2019 (COVID-19) first emerged in Wuhan, China at the end of 2019. In Korea, incidence of the disease started to increase rapidly from February 2020, and in March 2020, the World Health Organization declared a pandemic [1]. The number of children younger than 15 years who visited emergency departments (EDs) has decreased since the beginning of the pandemic [2-4]. As per a United States report on the status of ED visits from March to April 2020, the major declines in the visits were reported in age of 10 years or younger (72%) and 11-14 years (71%) [5]. To assess the pandemic-associated decrease in ED visits, Pikoulis et al. [6] proposed indicators, such as waiting time, disease severity, and hospitalization rate.
The decline in ED visits may be related to the caregivers’fear of nosocomial infection during the pandemic. Indeed, in a U.S. survey conducted since the beginning of the pandemic, 80% of respondents were concerned about visiting EDs as either a patient or visitor [7]. However, the main cause is the reduction in infectious diseases due to thorough precaution [5,8,9]. In a children’s hospital in Hangzhou, China, respiratory virus-related visits decreased to 7%-24% after the pandemic [8]. During the pandemic, U.S. children aged 10 years or younger had reduced incidences of influenza (by 97%), otitis media (85%), certain other upper respiratory diseases (84%), respiratory manifestations (78%), and fever (72%) compared to those in the same period in 2019 [5].
The authors investigated the change in the number and severity of febrile children who visited a tertiary hospital ED. These features were compared to those of preceding years. In addition, we obtained information on the number of children who underwent cancellation (see definition in Data collection and analysis) and the rates of respiratory virus polymerase chain reaction (PCR) performance and its positivity.
Methods1. Study populationThe authors analyzed the data of children aged 15 years or younger who visited the ED of a tertiary hospital with fever, regardless of their temperature at the time of visit, as the main symptom from 2017 through 2020. The pandemic period was defined as from February through August 2020 because the former month was the starting point of increase in incidence of COVID-19. This study was approved by the institutional review board with a waiver for informed consent (IRB no. 2020-12-143).
2. Data collection and analysisAll relevant data were extracted from the electronic medical records. We identified the monthly number of overall and fever-related ED visits. Baseline characteristics included age (month), sex, temperature, and duration of fever (hour). The high severity was defined as the Korean Triage and Acuity Scale (KTAS) triage level 1-2 (resuscitation or emergent). Aside from this definition, we recorded the proportion of children with primary diagnoses classified as the “mild disease”by the notice from the Korean Ministry of Health and Welfare [10]. We obtained the ED length of stay (minute), and ED disposition, including hospitalization, discharge, cancellation, and transfer. Of these components of the disposition, the cancellation was defined as the leave of children without treatment. In the canceled children, we reviewed the same symptom-related return visits within 7 days of the initial visit during the pandemic. As per the hospital policy, febrile children were expected to return to the outpatient clinic within 7 days. The data were compared between the febrile children who visited the ED in 2017-2019 and those who did in 2020 (February through August, each year).
The number of children undergoing the respiratory virus PCR was confirmed. This PCR was performed using Allplex Respiratory Panel 1-3 (Seegene, Seoul, Korea) and FilmArray (BioFire, Salt Lake City, UT). Since March 2020, the latter method has been used mainly in the children who needed a shorter turnaround time for hospitalization.
3. Statistical analysisWe performed monthly comparisons using Microsoft Office Professional Plus 2016 (Microsoft Corporation, Redmond, WA). The chi-square tests were used to analyze the differences between the categorical variables, and the Mann-Whitney U tests or Student t-tests were used to compare the differences between the continuous variables depending on the data distribution. P < 0.05 was considered statistically significant. SPSS ver. 25.0 (IBM Corp., Armonk, NY) was used for all analyses.
Results1. Increase in rates of KTAS 1-2 and hospitalizationFrom February to August 2020, the number of children who visited the ED due to fever was 1,124, 45.9% of the number in the preceding years (Table 1). However, the ratio of fever-related and overall ED visits in 2020 was similar to that in the preceding years, and the hospitalization rate tended to increase (Fig. 1, Table 1). The median age of the children was higher in 2020 than in the preceding years. The median duration of fever in 2020 was 9 hours (interquartile range, 2-23), which was shorter than the 11 hours (3-27) in the preceding years (P = 0.002). However, the median duration in February 2020 was 12 hours, which was slightly longer than the 11 hours. The rate of KTAS 1-2 in 2020 was higher than those in the preceding years (2017-2019, 5.7% vs. 2020, 16.4%; P < 0.001). In addition, the rate of mild diseases was lower in 2020. Hospitalization rate in 2020 was higher than that in the preceding years (2017-2019, 23.5% vs. 2020, 35.7%; P < 0.001). The hospitalization rate to the intensive care unit in 2020 was 0.6% (7 of the 1,124 children), which was higher than the 0.2% (12/7,352) in 2017-2019 (Table 1).
2. CancellationIn 2020, we noted 191 canceled children, accounting for 17.0% of the febrile children who visited in the year. The canceled children included those who visited only for severe acute respiratory syndrome- coronavirus 2 (SARS-CoV-2) testing and those who were sent to the COVID-19 screening center. The rate of KTAS 1-2 in 2020 tended to be lower than those in the preceding years. Major reasons for cancellation in 2020 were the guardians’ requests for discharge to avoid long waiting or being considered“ non-emergency”by medical staff (Table 2). Appendix 1 details the 7 children who were hospitalized after the initial cancellation in 2020. Of the 7 hospitalized children, a 45-month-old girl underwent a long waiting-related cancellation against a strong recommendation for treatment due to the 11-day history of fever. Later, she was diagnosed with leukemia.
3. PCRIn 2020, 344 children (30.6%) underwent respiratory virus PCR (Table 1). Fig. 2. depicts the sudden decrease in positive rate in March 2020 after the similar trend from 2017 through February 2020. The SARS-CoV-2 testing was performed in the 492 febrile children (43.8%), and none of them had positivity.
DiscussionThis study shows that the number of overall visits to the ED of a Korean tertiary hospital sharply decreased during the COVID-19 pandemic. This decrease has been experienced in many countries according to the studies during the pandemic [11,12]. Despite the decrease in overall visits, higher severity and hospitalization rates were shown in an analysis of all children who visited a U.S. ED over a 10-week period at the beginning of the pandemic [13]. In our study, the proportion of high severity (i.e., KTAS 1-2) increased while that of the mild disease decreased. Additionally, this study shows an increased cancellation rate during the pandemic, similar to the findings of a U.S. study [11]. The high rate of KTAS 1-2 in the canceled children in 2017-2019 might reflect frequent transfers to other hospitals of severely ill children. A lower severity of the canceled children in 2020 indicates that the ED was operated mainly for severely ill patients through the efficient triage, suggesting a proper function of the tertiary hospital ED during the pandemic.
The duration of fever in 2020 was shorter than in the preceding years. However, an Italian study reported in March 2020 showed the delayed visits of 12 severely ill children: 6 went to the intensive care unit, and 4 died [14]. In ours, the duration of fever in February 2020 was longer than before. Given the relatively earlier outbreak in Korea, the delayed visits at the early pandemic may be related to the guardians’concern about the nosocomial exposure to SARS-CoV-2. Also, the visits may have been delayed because there were insufficient facilities for infectious disease care due to the initial closure of medical facilities, or because the guardians had burden of caring for other children due to the closure of schools [15]. After the early pandemic, we noted decreases in the duration of fever and the mean temperature.
From March 2020, the study hospital additionally has used the FilmArray for respiratory virus PCR to make a quick decision and to increase the bed turnover during the pandemic. Even though the number of PCR has increased due to the quick method, the positive rate of viruses has decreased during the pandemic. Compared to the existing PCR, the FilmArray method is more expensive, faster, and as accurate [16]. A Chinese report showed a significant decrease in the detection of respiratory syncytial virus, influenza, and adenovirus since the pandemic [8]. As seen from the older median children’s age during the pandemic, the overall decrease in ED visits may be attributable to a decreasing incidence of respiratory viral diseases in younger children. The decrease may also be associated with the fear of nosocomial exposure to SARS-CoV-2 of guardians of children with low severity.
The first limitation of this study is the single-center study setting. The authors did not account for changes in government policy for COVID-19 and institutional policy for febrile patients. Given the retrospective design, we could not adjust for several confounding factors, such as the risk of COVID-19 or the severity of individual children, which may affect the reasons for ED visits. Additionally, the study population comprised only febrile children who previously accounted for the majority of pediatric patients. It may be necessary to investigate various disease groups, such as diabetes, as its incidence has increased among children due to the pandemic-related lifestyle changes [17].
This study shows that during the COVID-19 pandemic, febrile children’s visits to EDs may decrease while their severity, in terms of rates of KTAS 1-2 and hospitalization, may remain unchanged or increase. Since COVID-19 has allowed the ED of a tertiary hospital to function properly, it is vital to screen for severely ill children, and immediately treat them in separate rooms. Additionally, this finding can be useful for optimizing the diversion of the emergency medicine resources toward children with possible COVID-19 or other more urgent conditions.
Fig. 1.Annual trend of the febrile children’s visits to the emergency department. Despite the overall decrease in the total numbers of the visits, no such change was found in the ratio of fever-related and overall emergency department visits. In early 2020, the increases were noted in the rates of hospitalization and the KTAS 1-2. The respiratory virus PCR was performed in 39.3%-50.3% in 2017, 33.8%-56.7% in 2018, and 21.9%-49.7% in 2019. During the pandemic, the detection rate decreased to 3% until April 2020, then increased to 14%-18%. COVID-19: coronavirus disease 2019, PCR: polymerase chain reaction, KTAS: Korean Triage and Acuity Scale. 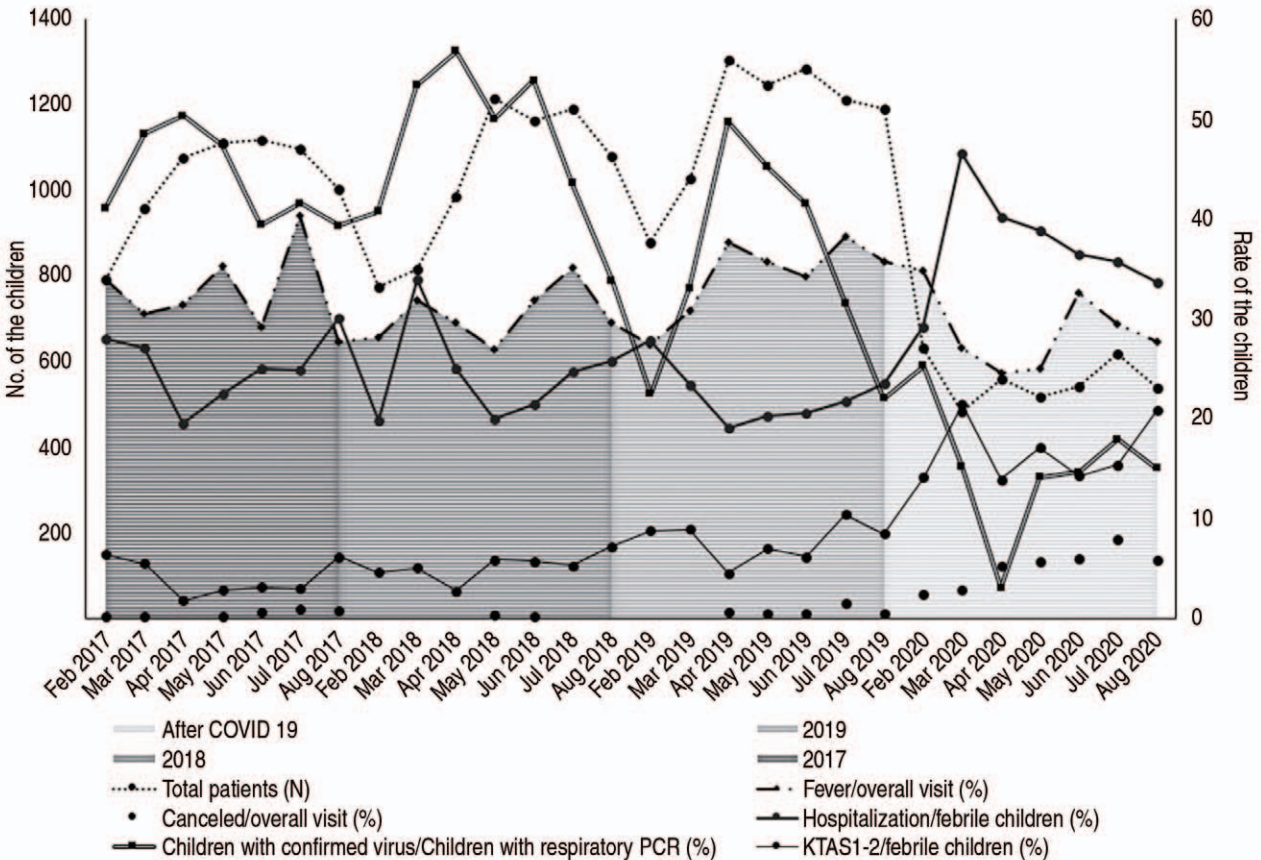
Fig. 2.Type and number of the confirmed respiratory viruses. The cumulative bars indicate the numbers of individual viruses. The line represents the numbers of children with 1 or more viruses. RSV: respiratory syncytial virus, COVID-19: coronavirus disease 2019. 
Table 1.Characteristics of the study population
Table 2.Characteristics of the canceled children
References1. Korean Society of Infectious Diseases, Korean Society of Pediatric Infectious Diseases, Korean Society of Epidemiology, Korean Society for Antimicrobial Therapy, Korean Society for Healthcare-associated Infection Control and Prevention, Korea Centers for Disease Control and Prevention. Report on the epidemiological features of coronavirus disease 2019 (COVID-19) outbreak in the Republic of Korea from January 19 to March 2, 2020. J Korean Med Sci 2020;35:e112.
2. Baugh JJ, White BA, McEvoy D, Yun BJ, Brown DFM, Raja AS, et al. The cases not seen: patterns of emergency department visits and procedures in the era of COVID-19. Am J Emerg Med 2020 Nov 5 [Epub]. https://doi.org/10.1016/j.ajem.2020.10.081.
3. Thornton J. COVID-19: A&E visits in England fall by 25% in week after lockdown. BMJ 2020;369:m1401.
4. Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes 2020;13:e006631.
5. Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, et al. Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019- May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:699–704.
6. Pikoulis E, Solomos Z, Riza E, Puthoopparambil SJ, Pikoulis A, Karamagioli E, et al. Gathering evidence on the decreased emergency room visits during the coronavirus disease 19 pandemic. Public Health 2020;185:42–3.
7. American College of Emergency Physicians. American College of Emergency Physicians COVID-19 [Internet]. Irving (TX): American College of Emergency Physicians: c2020 [cited 2020 Dec 1]. Available from: https://www.emergencyphysicians.org/globalassets/emphysicians/all-pdfs/acepmc-covid19-april-poll-analysis.pdf.
8. Li H, Yu G, Duan H, Fu J, Shu Q. Changes in children’s healthcare visits during coronavirus disease-2019 pandemic in Hangzhou, China. J Pediatr 2020;224:146–9.
9. Angoulvant F, Ouldali N, Yang DD, Filser M, Gajdos V, Rybak A, et al. Coronavirus disease 2019 pandemic: impact caused by school closure and national lockdown on pediatric visits and admissions for viral and nonviral infectionsa time series analysis. Clin Infect Dis 2021;72:319–22.
10. Korean Ministry of Health and Welfare. >Use a local clinic to treat mild diseases, such as otitis media, corns, and conjunctivitis! Sejong: Korean Ministry of Health and Welfare: 2019[cited 2020 Dec 1]. Available from: https://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=1&CONT_SEQ=346490. Korean.
11. Westgard BC, Morgan MW, Vazquez-Benitez G, Erickson LO, Zwank MD. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann Emerg Med 2020;76:595–601.
12. Choi DH, Jung JY, Suh D, Choi JY, Lee SU, Choi YJ, et al. Impact of the COVID-19 outbreak on trends in emergency department utilization in children: a multicenter retrospective observational study in Seoul metropolitan area, Korea. J Korean Med Sci 2021;36:e44.
13. Chaiyachati BH, Agawu A, Zorc JJ, Balamuth F. Trends in pediatric emergency department utilization after institution of coronavirus disease-19 mandatory social distancing. J Pediatr 2020;226:274–277. e1.
14. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health 2020;4:e10–1.
15. Chanchlani N, Buchanan F, Gill PJ. Addressing the indirect effects of COVID-19 on the health of children and young people. CMAJ 2020;192:E921–7.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

 |
 |