 |
 |
AbstractIn diabetic ketoacidosis, hyperglycemia and ketosis result in cerebral vasculitis, which can cause cerebral edema and thrombosis. A previously healthy, 12-year-old girl visited the emergency department with a history of vomiting, polydipsia, polyuria, decreased mentality, and a 7 kg (12%) weight loss within 1 week. She showed laboratory features of severe diabetic ketoacidosis, stuporous mentality, respiratory failure, and unilateral fixed mydriasis with contralateral hemiparesis. However, brain magnetic resonance imaging showed multifocal ischemic stroke mainly involving the left posterior cerebral artery territory, instead of uncal herniation. This case highlights the possible occurrence of ischemic stroke in children with early-stage diabetes mellitus.
IntroductionIn diabetic ketoacidosis (DKA), hyperglycemia and ketosis result in oxidative stress, increasing the secretion of inflammatory substances and eventually damaging the vascular endothelium, especially the intracerebral vessels[1]. Within a year of being diagnosed with type 1 diabetes mellitus, there is an increase in the inflammatory markers, such as tumor necrosis factor alpha or serum prothrombin fragment[2]. These mechanisms in DKA can lead to cerebral edema, uncal herniation, and ischemic stroke[3,4].
Approximately 3.5% of children with DKA show decreased mentality[5]. Thus, in children with DKA, it is vital to investigate the occurrence of cerebral complications. In this report, we detail a case of an adolescent girl with new-onset DKA with posterior cerebral artery (PCA) territory ischemic stroke with multifocal infarction. This study was approved by the institutional review board with a waiver for informed consent (IRB no. 2020-08-005).
CaseA previously healthy, 12-year-old girl visited the emergency department with decreased mentality, which occurred on the day of the visit. She also had a several-week history of polydipsia and polyuria, and 1-day history of vomiting. Moreover, there was a 7 kg (12%) weight loss within 1 week. The family history was noncontributory for diabetes mellitus.
The initial vital signs were as follows: blood pressure, 190/98 mmHg; heart rate, 90 beats per minute; respiratory rate, 30 breaths per minute; temperature, 36.6°C; and a Glasgow Coma Scale of 4. The height and weight were 160 cm (75-90 percentile) and 49.5 kg (50-75 percentile), respectively. She showed decreased skin turgor and dry oral mucosa.
Neurological examination showed unilateral fixed mydriasis (left pupil, 5 mm; right, 3 mm) and absent vestibulo-ocular reflexes. Further examination was limited due to the coma. The patient showed Kussmaul breathing in the emergency department. When she was hospitalized to the intensive care unit, the respiratory effort turned weak and shallow, leading to endotracheal intubation.
Initial serum glucose concentration was 490 mg/dL, and arterial blood gas analysis showed wide anion gap (18.6 mEq/L) metabolic acidosis with adequate respiratory compensation as follows: pH, 7.06; PCO2, 12.0 mmHg; and HCO3, 1.5 mmol/L. The results of the initial complete blood count were as follows: white blood cell count, 41,190/mm3; hemoglobin, 13.9 g/dL; and platelet count, 350,000/mm3. Other findings on chemistry and electrolytes were within the normal ranges. Urine ketone body was strongly positive. Consequently, DKA was diagnosed.
With a suspicion of potential uncal herniation given the unilateral fixed mydriasis, we performed brain magnetic resonance imaging (MRI) and angiography. The neuroimaging showed ischemic stroke of the left PCA territory (e.g., both uncus), left cerebellum, and splenium of the corpus callosum with mild cerebral edema (Fig. 1). There was no evidence of uncal herniation, visible thrombosis or vascular anomaly. Echocardiography showed no thrombus and structural abnormalities.
Acute management of DKA was implemented with hydration and intravenous insulin. Multifocal ischemic stroke was treated using mannitol, steroid (pulse therapy), and low-molecular-weight heparin. After hospitalization to the intensive care unit, the patient showed 1 episode of focal motor seizures involving the right arm and face. The seizures were controlled with lorazepam and fosphenytoin sodium. Electroencephalography showed disorganized background activity with diffuse sinusoidal slow waves without definite ictal findings. Surgical decompression was not performed given the inapparent cerebral edema with uncal herniation.
On day 2, the Glasgow Coma Scale changed to 7. As her mentality improved, motor response to pain was visible only on the right arm. After the motor response, the right leg began to move, and with a rehabilitation, all extremities began to respond to pain. On day 14, consciousness improved to alert; however, she showed an abnormal orientation, sleep disturbances, irritability, regression, and frequent crying out of context. One-month follow-up MRI showed partial resolution of the ischemic stroke (Fig. 2). At this time, her motor function was almost recovered.
DiscussionThe incidence of stroke ranges from 2 to 13 per 100,000 children[6]. It is known that 0.3%-1.0% of children with DKA show cerebral complications[7]. Stroke accounts for 10% of intracerebral complications in DKA patients[8]. Previous studies have associated stroke in DKA patients with vasculitis and coagulopathy given the oxidative stress-induced systemic inflammatory response[4]. When the patients present with decreased mentality, neurologic examination may be limited. Hence, it is vital to consider the stroke and relevant neuroimaging, such as MRI.
Uncal herniation secondary to cerebral edema can compress the PCA, incurring the ischemic stroke of the corresponding territory. Initially, unilateral fixed mydriasis in the case patient suggested uncal herniation, prompting MRI[9]. The MRI showed ischemic stroke involving the left PCA territory, left cerebellum, and splenium of the corpus callosum with minimal cerebral edema. However, no uncal herniation was observed. We speculated that a cerebral vasculitis caused the stroke involving the uncus. This uncal involvement was a probable cause of the neurologic manifestations without an uncal herniation.
The standard treatment for ischemic stroke has not yet been established. Some case reports show the use of tissue plasminogen activator or low-molecular-weight heparin, and warfarin in acute phase of the stroke[10,11]. Although magnetic resonance angiography showed no visible thrombus in the case patient, warfarin was administered given the presence of multifocal stroke including the PCA territory. After this anticoagulation, the stroke improved.
In comatose children with DKA, risk of intracerebral complications is often overlooked due to their decreased capability of communication. Thus, the risk needs more clinical attention. If neurological abnormalities are present, neuroimaging is essential. With the imaging, it is important to detect critical complications, such as uncal herniation requiring emergency decompression. Rapid diagnosis and treatment improve the outcome. Seizures should be controlled to prevent secondary brain damage.
In conclusion, we reported a 12-year-old girl with new-onset DKA with PCA territory ischemic stroke with multifocal infarction. Her neurologic manifestations were initially presumed to be secondary to cerebral edema-related uncal herniation. However, the manifestations were found to stem from the cerebral vasculitis-associated ischemic stroke.
Fig. 1.Findings of magnetic resonance imaging performed on day 1 (A-C, diffusion weighted image; D-F, apparent diffusion coefficient). Multifocal acute ischemic stroke is seen on the left occipital lobe (high and low signal intensities on diffusion weighted image [A, arrow] and apparent diffusion coefficient [D, arrow], respectively), both medial temporal lobes (uncus) and the right occipital lobe (B and E, arrows), and the left cerebellum (C and F, arrows). The left occipital lobe and ipsilateral medial temporal lobe belong to the left posterior cerebral artery territory. 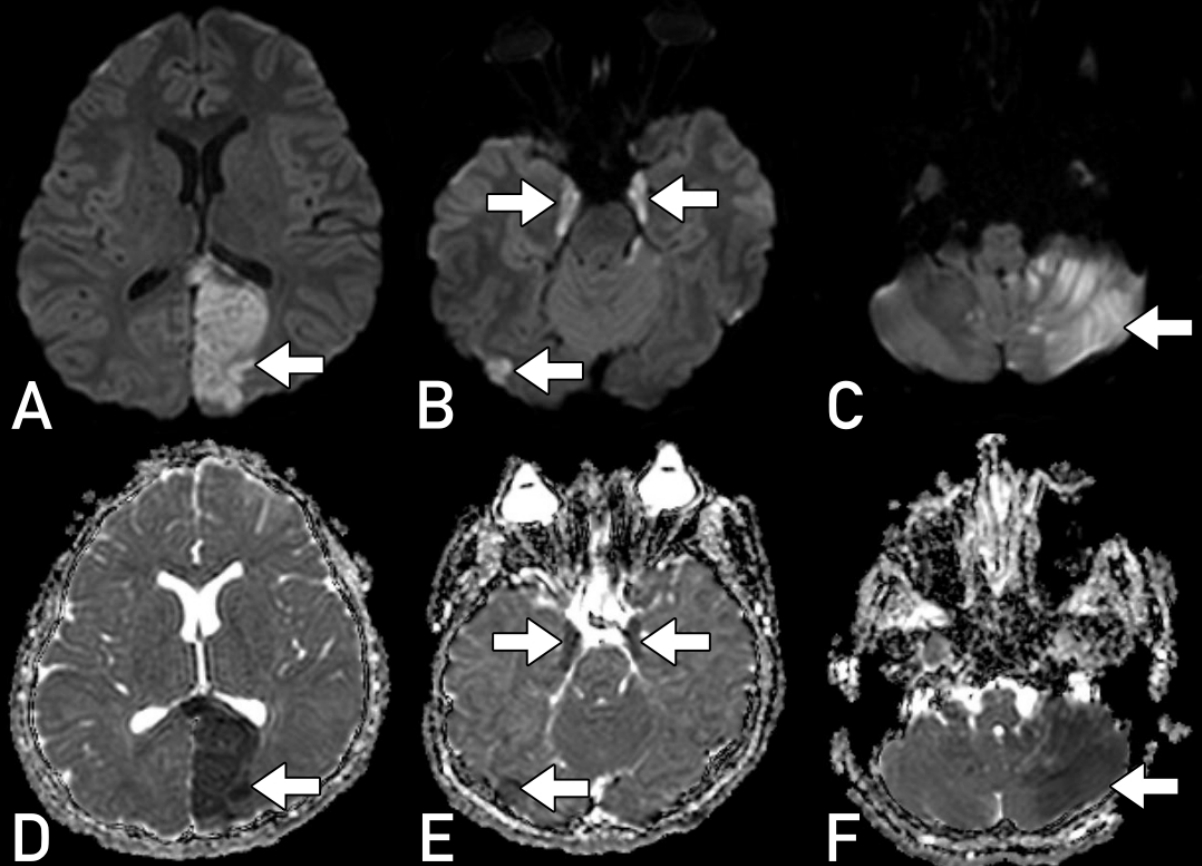
Fig. 2.Findings of 1-month follow-up magnetic resonance imaging (A-C, diffusion weighted image; D-F, apparent diffusion coefficient). The acute lesions are observed to be resolving (A, arrow). The high signal intensity on apparent diffusion coefficient refers to a chronic lesion (F, arrow). The majority of the cerebellar lesions were accompanied by atrophy while the lesions of posterior cerebral artery territory and most of the other cerebral lesions improved with a partial atrophy. 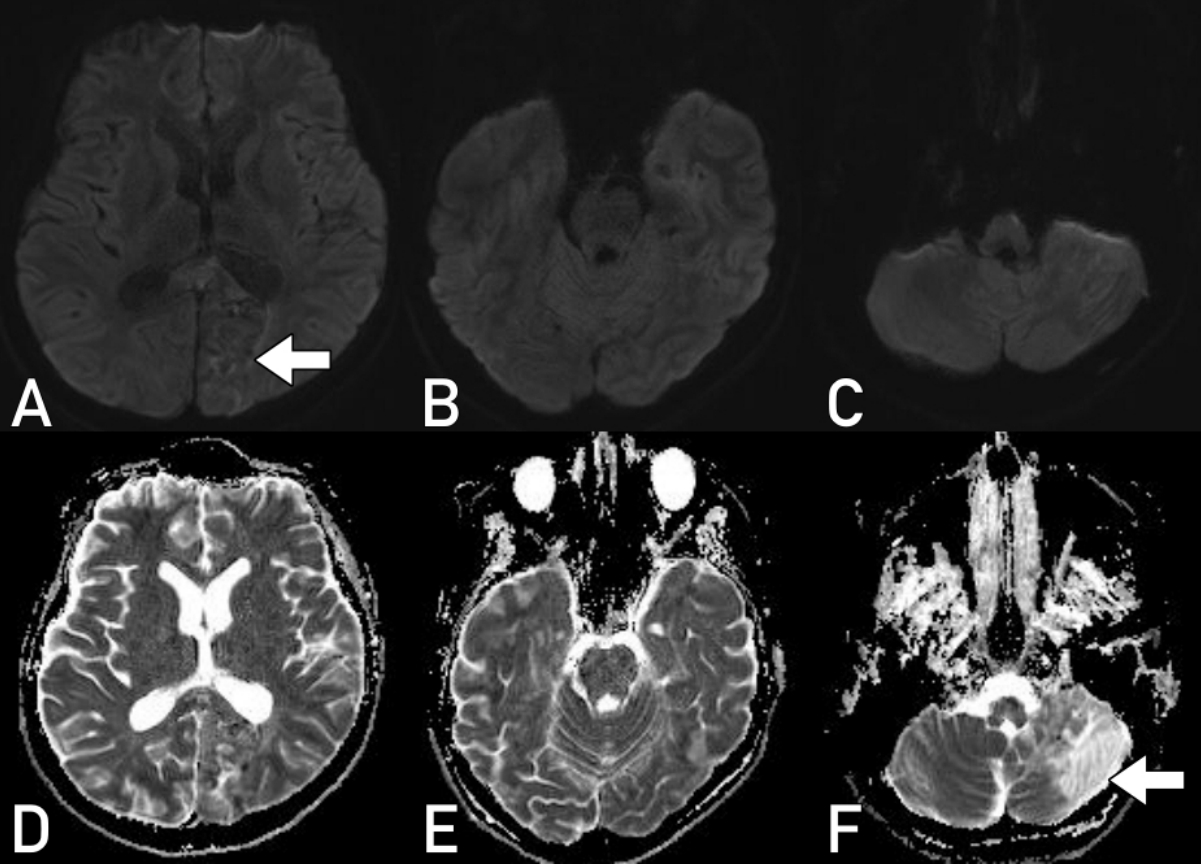
References1. Jain SK, McVie R, Bocchini JA. Hyperketonemia (ketosis), oxidative stress and type 1 diabetes. Pathophysiology 2006;13:163вАУ70.
2. Romano M, Pomilio M, Vigneri S, Falco A, Chiesa PL, Chiarelli F, et al. Endothelial perturbation in children and adolescents with type 1 diabetes: association with markers of the inflammatory reaction. Diabetes Care 2001;24:1674вАУ8.
3. Lawrence SE, Cummings EA, Gaboury I, Daneman D. Population-based study of incidence and risk factors for cerebral edema in pediatric diabetic ketoacidosis. J Pediatr 2005;146:688вАУ92.
4. Foster JR, Morrison G, Fraser DD. Diabetic Ketoacidosis-Associated Stroke in Children and Youth. Stroke Res Treat 2011;2011:219706.
5. Kuppermann N, Ghetti S, Schunk JE, Stoner MJ, Rewers A, McManemy JK, et al. Clinical trial of fluid infusion rates for pediatric diabetic ketoacidosis. N Engl J Med 2018;378:2275вАУ87.
6. Lynch JK, Hirtz DG, DeVeber G, Nelson KB. Report of the National Institute of Neurological Disorders and Stroke workshop on perinatal and childhood stroke. Pediatrics 2002;109:116вАУ23.
7. Ho J, Pacaud D, Hill MD, Ross C, Hamiwka L, Mah JK. Diabetic ketoacidosis and pediatric stroke. CMAJ 2005;172:327вАУ8.
8. Rosenbloom AL. Intracerebral crises during treatment of diabetic ketoacidosis. Diabetes Care 1990;13:22вАУ33.
9. Munakomi S, M Das J. Brain herniation. In: StatPearls [Internet] Treasure Island (FL): StatPearls Publishing: c2020 [cited 2020 Aug 6]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK542246/.
10. Shuayto MI, Lopez JI, Greiner F. Administration of intravenous tissue plasminogen activator in a pediatric patient with acute ischemic stroke. J Child Neurol 2006;21:604вАУ6.
11. Roach ES, Golomb MR, Adams R, Biller J, Daniels S, Deveber G, et al. Management of stroke in infants and children: a scientific statement from a Special Writing Group of the American Heart Association Stroke Council and the Council on Cardiovascular Disease in the Young. Stroke 2008;39:2644вАУ91.
|
|
|||||||||||||||||||||||||||||||||||

 |
 |