 |
 |
AbstractPurposeTo develop a clinical scoring system for children with presumed appendicitis who visit the emergency department.
MethodsA registry based-retrospective study was conducted in the pediatric emergency department between September 2015 and December 2016. Patients aged 4 to 17 years who had a > 1 of 5 Likert scale for possibility of appendicitis were included. Multiple logistic regressions based on Akaike information criterion were performed using variables regarding clinical features and inflammatory markers to develop the clinical scoring system.
ResultsA total of 233 patients were included, and 93 (39.9%) had the final diagnosis of appendicitis. The final model with the lowest Akaike information criterion (171.7) consisted of 5 variables, including vomiting (1 point), absence of watery diarrhea (1 point), duration of symptoms Ōēż 3 days (1 point), rebound tenderness (1 point), and white blood cell count > 10.0 ├Ś 109/L (2 points). If the clinical score was Ōēź 4 of 6 points, the area under the receiver operating characteristic curve was 0.78 (95% confidence interval, 0.71-0.86) with a 78.9% sensitivity, 66.7% specificity, positive and negative predictive values of 70.0% and 76.2%, respectively, and positive and negative likelihood ratios of 2.4 and 0.3, respectively.
IntroductionAcute appendicitis is traditionally predicted based on clinical features and laboratory results. Recent advances in imaging techniques have led to the use of ultrasound (US) and computed tomography (CT) prior to operation in many countries [1-3]. Increasing use of CT can reduce the rate of negative appendectomy [4]. However, some authors suggest that CT does not significantly reduce the rate of negative appendectomy among children [5]. Moreover, the use of CT in young children could increase potentially unnecessary radiation exposure and use of sedatives [6]. Various clinical pathways for predicting pediatric appendicitis have been proposed to reduce the need for unnecessary CT [7,8]. Although the Alvarado score and Pediatric Appendicitis Score (PAS), which consisted of symptoms, signs, and inflammatory markers, were developed as diagnostic tools for acute appendicitis, the validity was not evaluated by well-designed studies [9-11].
However, no clinical scoring systems or clinical decision rules have been developed in the Korean pediatric emergency department (ED) environment. The purpose of this study was to develop a clinical scoring system for appendicitis in children presumed to have it who visit the ED.
Methods1. Study design and settingThis study was a prospectively collected registry-based retrospective study to develop a clinical scoring system for pediatric appendicitis. It was conducted at a tertiary care, university-affiliated hospital pediatric ED in Seoul, Korea, having which has approximately 20,000 visits annually. Patients aged 4-17 years who visited the ED from September 2015 to December 2016 were considered eligible. Children presumed to have appendicitis were registered in the Pediatric Suspected Appendicitis Registry. Physicians evaluated the possibility of appendicitis with 5-point Likert scale before imaging tests. We excluded the patients who had a 0-1 point of the scale. The institutional review board approved this study (IRB no. 1806-165-953).
2. Data variablesAll enrolled patients were divided into the appendicitis group and the non-appendicitis group based on the final diagnosis. All clinical features and inflammatory markers were routinely collected through the registry during the ED stay, and were compared between the 2 groups. The final diagnosis was based on pathology reports if available. If there was a follow-up medical report in non-operated patients, we contacted them via telephone within 1 month after the ED visit. The non-appendicitis group consisted of patients who had other diagnoses in the ED or at follow-up visits, those who did not return to the hospital as scheduled, and those who were not contactable.
We collected the following variables: age (years), sex, duration of symptoms (Ōēż 3 days), fever (Ōēź 38Ōäā in the ED or at home), anorexia, nausea, vomiting, absence of watery diarrhea, migration of pain to the right lower quadrant (RLQ), RLQ tenderness, rebound tenderness, muscle guarding, inflammatory markers (white blood cell [WBC] count, neutrophil ratio > 75%, and C-reactive protein [CRP]), imaging results (CT and US) as both continuous and categorical variables, and final diagnosis (as aforementioned).
3. Development of a clinical scoring system for pediatric appendicitisAkaike information criterion (AIC)-based logistic regression analysis was performed to develop a clinical scoring system for pediatric appendicitis using variables having P < 0.200. AIC was applied to compare the difference of models, and adopted as a criterion for evaluating prognostic performance of prediction models. When the AIC value is lower, the model goodness of fit is better [12,13]. The model with the minimum AIC value was selected. We developed a clinical scoring system using the adjusted ╬▓ coefficients from the final model, multiplying them by a patientŌĆÖs own values for the corresponding variables, and then summing over the resulting set of products to arrive at a patient-specific final score. Thus, this final score represented the sum of a patientŌĆÖs risk factors, with each factor weighted by its predictive ability in the multivariable model. The area under the receiver operating characteristic curves was calculated to evaluate the performance of the developed score, cutoff values were obtained according to YoudenŌĆÖs index (J = max [sensitivity + specificity ŌĆō 1]), and sensitivity, specificity, positive and negative predictive values, and likelihood ratios (LRs) were calculated. The performance of our scoring system was compared with those of the Alvarado score and the PAS using DeLong test [9,10].
4. Statistical analysisClinical features were examined using a chi-square test or Fisher exact test for categorical variables and Mann-Whitney U test for continuous variables, respectively. The sample size was estimated using the ŌĆ£event per variableŌĆØ based on findings from empirical simulation with logistic regression [14]. Based on the 8 predictors of the previous tools [9,10], we estimated that 90 patients with appendicitis were needed to avoid the overfitting multivariable model considering a 10% dropout rate. The rate of appendicitis was reported to be 38% in this registry, and the sample size was 239. All statistical analyses were conducted using IBM SPSS Statistics version 20 (IBM Corp, Armonk, NY) and R version 3.4.3 (http://www.r-project.org). A P < 0.050 was considered statistically significant.
Results1. Clinical features of the study populationOf the 239 patients enrolled in the registry, 233 were assigned 2-5 points in Likert scale. The median age was 10 (interquartile range, 7-13) years, and men comprised 53.6% of the patients. Ninety-three patients (39.4%) were designated as the appendicitis group. As first imaging modality, US and CT were performed in 78.1% (182 of the 233 patients) and 20.2% (47 of the 233 patients), respectively. No differences were found in the frequency of the imaging tests between the 2 groups (P = 0.346) (Fig. 1). In the univariate analysis, the variables having P < 0.200 were sex, duration of symptoms within 3 days, anorexia, vomiting, absence of watery diarrhea, migration of pain to the RLQ, rebound tenderness, muscle guarding, WBC > 10.0 ├Ś 109/L, CRP > 1 mg/dL, neutrophil ratio > 75% (Table 1). Among the patients with 1 point in Likert scale, no one had appendicitis.
2. Development of a clinical scoring system for pediatric appendicitisLogistic regression analysis selected the final model (AIC = 171.7) with 5 variables including vomiting, absence of watery diarrhea, duration of symptoms Ōēż 3 days, rebound tenderness, and WBC > 10.0 ├Ś 109/L. Using the estimate value of each variable, a clinical scoring system for appendicitis was developed and multiplied by 1 point for each variable except the WBC (multiplied by 2 points) (Table 2). The clinical scoring system calculation formula is as follows.
A clinical scoring system = (vomiting ├Ś 1) + (absence of watery diarrhea ├Ś 1) + (duration of symptoms Ōēż 3 days ├Ś 1) + (rebound tenderness ├Ś 1) + ([WBC > 10.0 ├Ś 109/L] ├Ś 2)
The probability of appendicitis according to each score of the clinical scoring system is shown in Fig. 2. The cutoff value was 4 points, and sensitivity, specificity, positive predictive value, negative predictive value, positive LR, and negative LR were 78.9%, 66.7%, 70.0%, 76.2%, 2.37, and 0.32, respectively (Table 3). The performance of the clinical scoring system was better than those of the Alvarado score and the PAS (Fig. 3). There were no patients with appendicitis at 0 point, 9 at 1 point, 4 at 2 points, and 21 at 3 points. The 9 patients who had the clinical score of 1 point were negative in all but the duration of symptom Ōēż 3 days. Two of the 4 patients who had the clinical score of 2 were positive for the vomiting and duration of symptoms Ōēż 3 days, 1 of them was positive for the duration of symptoms Ōēż 3 days and rebound tenderness, 1 of them was positive for the absence of watery diarrhea and duration of symptoms Ōēż 3 days.
DiscussionWe developed a 5-item clinical scoring system that shows a fair performance in predicting pediatric appendicitis. Imaging tests for appendicitis could be recommended if the score is 4-6 points. Patients with the score of 0-3 points could undergo a follow-up physical examination or be discharged, rather than have an unnecessary CT scan performed. Clinician can use this tool easily since the number of variables is smaller than those of the Alvarado score and the PAS [9,10].
In the present study, the significant variables consisted of 3 symptoms, 1 sign, and 1 inflammatory marker. The Alvarado score has 6 clinical variables and 2 laboratory measurements with the total of 10 points, and the PAS has the same variables with different scoring system [9,10]. Among the variables used in these 2 scoring systems, anorexia, fever, RLQ tenderness, and migration of pain to the RLQ were not significant in this study [9,10]. This difference might be due to the fact that the study patients were presumed to have appendicitis, and they make up only a portion of children with abdominal pain. Patients with the score of 4-6 points may have at least 40% possibility of acute appendicitis. The insignificance of the RLQ tenderness might be due to the similarly high frequencies in both groups (86.0% vs. 84.2%).
Contrary to the well-known clinical scoring system [9,10], this scoring system includes the absence of watery diarrhea. O'Shea et al. [15] reported that this variable had a 33% sensitivity, 87% specificity, positive LR of 2.55 (95% confidence interval [CI], 1.32-4.94) and negative LR of 0.77 (95% CI, 0.58-1.02). Another study showed a 22% sensitivity, 82% specificity, positive LR of 1.21 (95% CI, 0.84-1.75) and negative LR 0.95 (95% CI, 0.87-1.05) [16]. Interestingly, the absence of watery diarrhea was chosen as a variable in this study because watery diarrhea is a common symptom in enterocolitis, which should be distinguished.
There have been many reports on the duration of symptoms of acute appendicitis. Similar to our study, Bachur et al. [17] reported a 5% sensitivity, 89% specificity, positive LR of 0.31, and negative LR of 1.08, when the duration of symptoms exceeded 72 hours. A meta-analysis shows that the symptom duration of 12-24 hours was the best with pooled data of a 35% sensitivity (95% CI, 30-40) and 69% specificity (95% CI, 67-71) compared to the other symptom periods [18].
Of the inflammatory markers, WBC > 10.0 ├Ś 109/L was assigned a higher score than other variables. Contrary to WBC and CRP, new inflammatory markers, such as calprotectin and proadrenomedullin, are unavailable in most institutions [19,20]. Thus, a new clinical scoring system that includes WBC can be applied to settings with limited resources.
Vomiting is a common and nonspecific symptom in children presenting to the ED. It could be due to abdominal, infectious or neurologic diseases. As a symptom of appendicitis, vomiting was included in the Alvarado and the PAS [15,16]. Our clinical scoring system also includes vomiting as a variable.
This study has several limitations. First, this current study was carried out in a single center with a relatively small sample size. Thus, it may be difficult to apply this scoring system in different settings. Second, the expertise level of doctors who enrolled the patients to the registry varied from junior residents to attending physicians. However, this variety may reflect the practice patterns at tertiary care hospital EDs. Third, it was difficult to contact all patients after discharge. Having appendicitis was less likely in the patients who was not diagnosed with it, and did not return to this hospital after discharge, since most patients who have problems after discharge are likely to return to the tertiary care hospital ED. Fourth, since the study was conducted retrospectively based on prospectively-collected registry data with missing values in some variables, it is necessary to validate the clinical scoring system.
We developed a simple clinical scoring system to predict appendicitis in children presumed to have it who visit the ED. This scoring system may help reduce unnecessary use of CT in the children at relatively low risk for appendicitis.
Fig.┬Ā1.Comparison of imaging tests between the appendicitis group and the non-appendicitis group. The rates of ultrasound (US) only, computed tomography (CT) only, and US and CT were 61.3% (57 of the 93 patients), 21.5% (20 of the 93 patients), and 17.2% (16 of the 93 patients), respectively, in the appendicitis group, and they were 59.3% (83 of the 140 patients), 17.9% (25 of the 140 patients), and 20.0% (28 of the 140 patients), respectively, in the non-appendicitis group. The differences between the 2 groups were insignificant (P = 0.346). 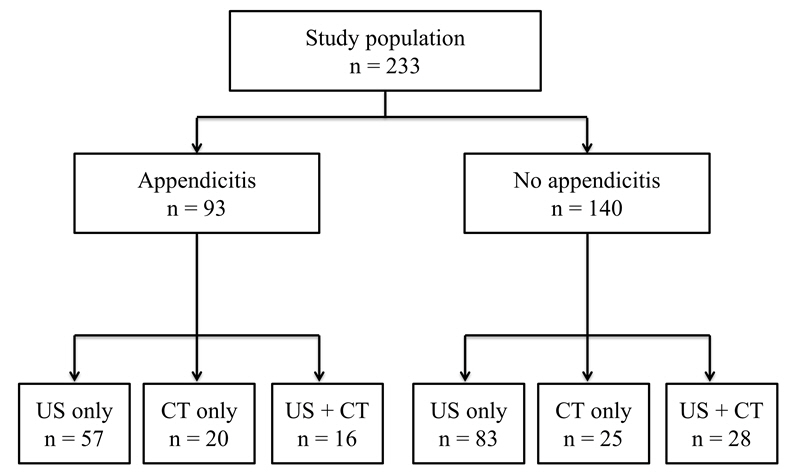
Fig.┬Ā2.Predicted probability of appendicitis according to each score of a clinical scoring system. When the score increased from 0 to 6, the predicted probabilities were 5.0%, 10.7%, 21.4%, 38.2%, 58.5%, 76.2%, and 87.9%, respectively. Of note, a patient with score of 4 points had an approximately 40% probability. 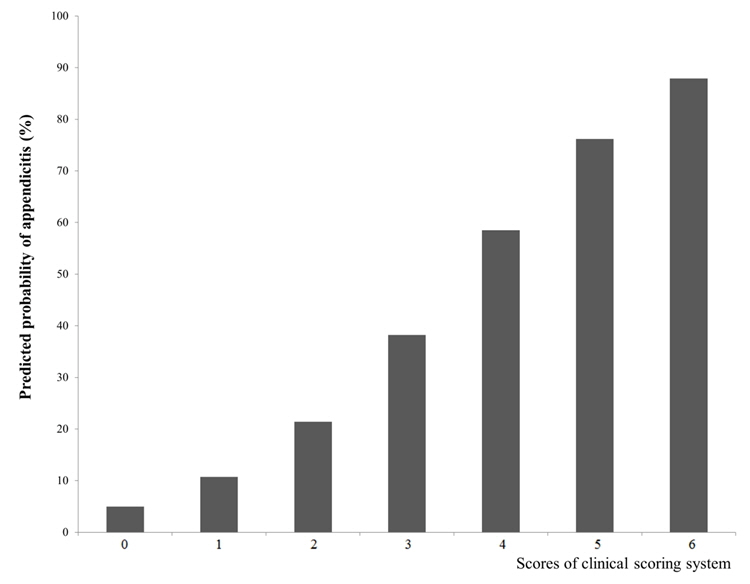
Fig.┬Ā3.Comparison of performance of a clinical scoring system, the Alvarado score, and the Pediatric Appendicitis Score (PAS). The area under the receiver operating characteristic curves of the clinical scoring system (solid line) was bigger than those of the Alvarado score [15] and the PAS [16] (0.78 [95% CI, 0.71-0.86] vs. 0.71 [95% CI, 0.63-0.80] and 0.68 [95% CI, 0.57-0.75], respectively; P < 0.001). CI: confidence interval. 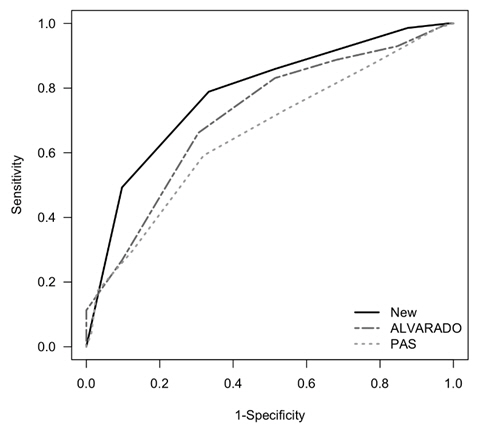
Table┬Ā1.Clinical features of the study patients
Table┬Ā2.Logistic regression based on Akaike information criterion (AIC)*
Table┬Ā3.Performance of the clinical scoring system for pediatric appendicitis
* If the clinical score was Ōēź 4 of 6 points, the area under the receiver operating characteristic curve was 0.78 (95% confidence interval, 0.71-0.86) with a 78.9% sensitivity, 66.7% specificity, positive and negative predictive values of 70.0% and 76.2%, respectively, and positive and negative LRs of 2.4 and 0.3, respectively. References1. Lahaye MJ, Lambregts DM, Mutsaers E, Essers BA, Breukink S, Cappendijk VC, et al. Mandatory imaging cuts costs and reduces the rate of unnecessary surgeries in the diagnostic work-up of patients suspected of having appendicitis. Eur Radiol 2015;25:1464ŌĆō70.
2. Boonstra PA, van Veen RN, Stockmann HB. Less negative appendectomies due to imaging in patients with suspected appendicitis. Surg Endosc 2015;29:2365ŌĆō70.
3. Bolmers MD, van Rossem CC, Gorter RR, Bemelman WA, van Geloven AAW, Heij HA, et al. Imaging in pediatric appendicitis is key to a low normal appendix percentage: a national audit on the outcome of appendectomy for appendicitis in children. Pediatr Surg Int 2018;34:543ŌĆō51.
4. Krajewski S, Brown J, Phang PT, Raval M, Brown CJ. Impact of computed tomography of the abdomen on clinical outcomes in patients with acute right lower quadrant pain: a meta-analysis. Can J Surg 2011;54:43ŌĆō53.
5. Martin AE, Vollman D, Adler B, Caniano DA. CT scans may not reduce the negative appendectomy rate in children. J Pediatr Surg 2004;39:886ŌĆō90.
6. Shah NB, Platt SL. ALARA: is there a cause for alarm? Reducing radiation risks from computed tomography scanning in children. Curr Opin Pediatr 2008;20:243ŌĆō7.
7. Wagenaar AE, Tashiro J, Wang B, Curbelo M, Mendelson KL, Perez EA, et al. Protocol for suspected pediatric appendicitis limits computed tomography utilization. J Surg Res 2015;199:153ŌĆō8.
8. Ramarajan N, Krishnamoorthi R, Barth R, Ghanouni P, Mueller C, Dannenburg B, et al. An interdisciplinary initiative to reduce radiation exposure: evaluation of appendicitis in a pediatric emergency department with clinical assessment supported by a staged ultrasound and computed tomography pathway. Acad Emerg Med 2009;16:1258ŌĆō65.
9. Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med 1986;15:557ŌĆō64.
11. Kulik DM, Uleryk EM, Maguire JL. Does this child have appendicitis? A systematic review of clinical prediction rules for children with acute abdominal pain. J Clin Epidemiol 2013;66:95ŌĆō104.
12. Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol 2007;165:710ŌĆō8.
13. Akaike H. Information theory as an extension of the maximum likelihood principle. 2nd ed. Petrov BN, Csaki F, editors. Second International Symposium on Information Theory Budapest (HU): Akademiai Kiado: 1973. p. 267ŌĆō81.
14. Peduzzi P, Concato J, Feinstein AR, Holford TR. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J Clin Epidemiol 1995;48:1503ŌĆō10.
15. O'Shea JS, Bishop ME, Alario AJ, Cooper JM. Diagnosing appendicitis in children with acute abdominal pain. Pediatr Emerg Care 1988;4:172ŌĆō6.
16. Santillanes G, Simms S, Gausche-Hill M, Diament M, Putnam B, Renslo R, et al. Prospective evaluation of a clinical practice guideline for diagnosis of appendicitis in children. Acad Emerg Med 2012;19:886ŌĆō93.
17. Bachur RG, Dayan PS, Bajaj L, Macias CG, Mittal MK, Stevenson MD, et al. The effect of abdominal pain duration on the accuracy of diagnostic imaging for pediatric appendicitis. Ann Emerg Med 2012;60:582ŌĆō90. e3.
18. Benabbas R, Hanna M, Shah J, Sinert R. Diagnostic accuracy of history, physical examination, laboratory tests, and point-of-care ultrasound for pediatric acute appendicitis in the emergency department: a systematic review and meta-analysis. Acad Emerg Med 2017;24:523ŌĆō51.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

 |
 |