 |
 |
AbstractPurposeThis study was performed to review the mortality pattern at the emergency ward (EW) of the Rivers State University Teaching Hospital, Port Harcourt, Nigeria.
MethodsA retrospective review of mortality among children hospitalized in the EW was conducted from January 2015 through May 2017. Information on their age, sex, weight, diagnosis, and mortality was recorded. The data were expressed in frequencies, and logistic regressions were performed with mortality as the dependent variable.
ResultsThe median age of the 1,020 children hospitalized in the EW was 1.0 year (interquartile range, 0.6-4.0) with death recorded in 60 children, a 5.9% mortality rate. Mortality was higher in the children younger than 2 years, boys, and those with infectious diseases. Of the 60 dead children, infectious diseases were the leading cause of mortality (53 [88.3%]) with sepsis (22 [36.7%]), gastroenteritis (10 [16.7%]), and meningitis (6 [10.0%]), accounting for the highest contributors to mortality. The highest case fatality rates were noted in tetanus (1/1 [100%]), human immunodeficiency virus (5/14 [35.7%]), and tuberculosis (2/7 [28.6%]). The logistic regression showed that age of 13-16 years (adjusted odds ratio, 4.59; 95% confidence interval, 1.80-11.20; compared with age < 2 years) and presence of infectious diseases (4.65; 1.80-12.10) significantly increased the risk of mortality.
IntroductionGlobally, there has been a remarkable improvement in children’s survival over the past 3 decades. However, continued efforts are required to further reduce their mortality rates because many children still die from preventable diseases, particularly in the developing countries1). Infectious diseases, such as pneumonia, diarrhea, and malaria, remain a leading cause of death in children younger than 5 years, along with preterm birth and intrapartum-related complications1).
Emergency units represent the first point of care for the critically ill children, and their death in emergency wards (EWs) is challenging to the clinicians or families who have to deal with it2). Mortality in EWs depends on geographic regions. In developed countries, mortalities have been reported to be below 1%3,4). In contrast, studies from developing countries have reported mortalities range from 2.8% to 4.1% among children hospitalized in EWs5,6). The mortality in Nigeria ranges from 2% to 13.6%7-9).
Worldwide variations have also been reported in the causes of death in EWs. Whereas trauma and cardiovascular diseases were important causes in developed countries3,4), infectious diseases predominate in the developing countries in sub-Saharan Africa7-9).
Factors associated with mortality in EWs vary among different authors. A Nigerian study reported that the mortality was higher in the first 24 hours of hospitalization and during the dry months of the year as well as in children younger than 3 years7,9). Other factors include low socioeconomic status, malnutrition, and a previous episode of diarrhea as reported in Ghana5).
It is vital to study the pattern of mortality in EWs. Such a study provides the trend and distribution of diseases, data for the planning of disease prevention and control programs, and an opportunity for the emergency care team to evaluate its standard of care and improve on areas of concern. The present study sought to analyze the mortality pattern among children hospitalized in the EW of the Rivers State University Teaching Hospital, Port Harcourt, southern Nigeria.
MethodsThis was a retrospective review of the patient register of the EW from January 2015 through May 2017. This study was approved by the hospital health research ethics committee (IRB no. RSUTH/REC/2022228). The emergency unit renders health care for all children aged 16 years or younger. All children seen in the emergency unit can either be hospitalized into the EW or the special care baby unit of the hospital if they are aged 28 days or younger while those not requiring hospitalization are discharged after their consults.
Data of all hospitalizations within the study period were entered into an Excel spreadsheet (Microsoft, Redmond, WA). Information on their age, age groups (< 2, 2-5, 6-12, and 13-16 years), sex, weight, diagnosis, and mortality was recorded. Diseases that occurred once or did not belong to any group were classified as others with exception of those in whom mortality occurred. A weight for age Z-score was used to classify nutritional status. The case fatality rate (CFR) was defined as the number of mortalities among those with diseases.
To determine risk factors for mortality, we performed multivariable logistic regressions with backward stepwise variable selection using mortality as the dependent variable. Variables with up to 20% missing data were excluded from being put into the model. Results were reported as adjusted odds ratios (aORs) and 95% confidence intervals (CIs). Data were analyzed using IBM SPSS ver. 23.0 for Windows (IBM Corp., Armonk, NY). Data distribution was also expressed in frequency tables and charts.
Results1. Description of mortalityThe number of children hospitalized during the study period was 1,020 with a median age of 1.0 year (interquartile range, 0.6-4.0). Mortality was recorded in 60 (5.9%). Among the age groups, children aged < 2 years showed the highest mortality of 66.7%, followed by those aged 6-12 years (9 [15.0%]) (Table 1). Mortality was higher in boys. Weights were not documented in 51.7% of the children with mortality. Among those with available weights, the majority of mortality occurred in those with normal weight (26.7%). Infectious diseases contributed to the majority of mortality in the EW (88.3%).
2. Diagnoses of the hospitalized children and their age distributionThe most common diagnosis was malaria (19.9%), followed by acute respiratory infection (17.7%), gastroenteritis (11.3%), sepsis (10.9%), and acute asthma (7.1%) (Table 2). The 180 children with acute respiratory infection consist of 100 with tonsillitis (9.8%), 66 with bronchopneumonia (6.5%), and 14 with bronchiolitis (1.4%). The 115 children with gastroenteritis consist of 106 with non-bloody diarrhea (10.4%) and 9 with dysentery (0.9%). Children younger than 2 years had a similar pattern of hospitalization as the overall population. In older children, the most common reason for hospitalization into the EW was acute asthma, as shown by 28 (16.9%) and 8 (18.2%) in those aged 6-12 years and aged 13-16 years, respectively.
3. Risk factors for mortalityAmong the age groups, the highest mortality of 15.9% (7 of the 44 children) was noted in the children aged 13-16 years. In univariable analysis, the age group’s mortality was higher than that of other groups (aOR, 2.75; 95% CI, 1.15-6.56; compared with age < 2 years) (Appendix 1; https://doi.org/10.22470/pemj.2022.00598). The mortality rate of the children aged 2-5 years was lowest among the age groups (1.5% [2 of the 137]). The type of disease and nutritional status significantly affected the mortality. The underweight children had a higher mortality of 12.8% (3.80; 1.68-8.36; compared with normal weight). Those with infectious diseases had a higher mortality rate of 7.3% (4.10; 1.68-10.47; compared with non-communicable diseases).
We performed the multivariable logistic regressions to ascertain the effect of age group and presence of infectious diseases (Table 3). The regression model was statistically significant (χ2 = 20.6, P < 0.001). It explained 59% of the variance observed in the mortalities and correctly classified 94% of the mortalities observed. Resultantly, independent factors associated with mortality were the age of 13-16 years (aOR, 4.59; 95% CI, 1.80-11.20; compared with age < 2 years) and the presence of infectious diseases (4.65; 1.80-12.10).
DiscussionIn the present study, the 5.9% mortality of children hospitalized to the EW was comparable with 5.1% and 6.2% reported respectively in Enugu10) and Umuahia11) of southeastern Nigeria, but higher than 4.1%, 3.9%, 2.5%, and 1.6% reported respectively in Ethiopia6), a more recent study in Enugu7), India12) and Mozambique13). However, the 5.9% was lower than 7.6%, 9.6%, 10.6%, 11.1%, and 11.6% documented in other regions of Nigeria14-16).
The varying mortalities are attributable to the difference in geographic regions or time, as observed in the studies in Enugu7,10). Of note, children in developing countries, especially in sub-Saharan Africa, still have a relatively high mortality, which is 14 times higher than the equivalent values in Europe and North America1). The high mortality could be attributed to poorly developed health policies, poor funding, inadequate manpower, and infrastructure. Other factors for high mortality in EWs are delayed visits, financial constraints due to the unavailability or lack of enforcement of the National Health Insurance Scheme, delayed interventions, and inadequate support services17). Hence, a multidisciplinary approach is needed to reduce childhood mortality in Port Harcourt, which is located in sub-Saharan Africa.
Seventy percent of the mortality in the EW was observed in the children aged 5 years or younger. This high mortality in the young children was also documented by other researchers7,10,14-16,18). This tendency may stem from this group being more prone to poor outcomes due to their immature immunity against common infections. Therefore, the finding prompts the implementation of already existing preventive measures for childhood diseases, and timely diagnosis and treatment.
Infectious diseases were responsible for over 75% of mortality in the present study. This finding corroborates studies in some regions of Nigeria7,10,14,16,19), and the Democratic Republic of Congo20), and reports by the World Health Organization stating infectious diseases as the leading cause of childhood mortality1,21). Contrary to the above studies, Jofiro et al.6) in Ethiopia reported cardiovascular and infectious diseases as the most and the third common cause of death, respectively. This disparity could be attributed to differences in the study population. The population in the Ethiopian study included neonates who have a higher prevalence of congenital heart diseases, unlike the other studies which excluded neonates6). It is notable that infectious diseases, common entities in sub-Saharan Africa, could be prevalent due to the combination of lack of immunization and low socioeconomic status.
The odds of mortality were about 5 times higher among the children aged 13-16 years, as well as among those with infectious diseases. Globally, mortality falls from the peak at age younger than 5 years to trough at age of 10-14 years, and increases again in older adolescents and young adults22). This increase in mortality stems from the fact that older adolescents are in a critical period of transition to adulthood. This period is associated with certain health risks, which lead to increased mortality23). The risks include road traffic accidents, abuse of alcohol or substance, risks in workplace, reproductive risks, and other non-communicable diseases. Thus, interventions to improve survival of older adolescents should be strengthened by multidisciplinary approaches, such as improvement of education, transportation, road infrastructure, and law enforcement.
Sepsis was the most common cause of death in the EW. This finding is consistent with the equivalent findings reported by Edelu et al.7), Enyuma et al.8), and Ndukwu and Onah18) in Enugu, Calabar, and Nnewi in Nigeria, respectively. In contrast, this finding is contrary to other regions in the country. In Aba and Bauchi, Nigeria, severe malaria was the leading cause of death whereas anemic heart failure was documented in Bayelsa14-16). In Ethiopia and Malawi, pneumonia was the leading cause of death6,24). Such differences may be related to the variations according to geographic regions, even in the same country, or over time.
CFR was highest in infectious diseases, such as tetanus (100%), human immunodeficiency virus (35.7%), and tuberculosis (28.6%), in the present study. Notably, the most common causes of death were also infectious diseases. Infectious diseases accounting for the highest CFR were also documented in a 4-year retrospective study in Umuahia where meningitis (28.6%), sepsis (17.1%), and malaria (3.3%) had the highest CFR19).
As a limitation, there were incomplete or missing data due to the retrospective study design. Thus, we encourage to use of an electronic health management system to store medical records in good condition.
The mortality of children hospitalized in the EW of the Rivers State University Teaching Hospital was 5.9% with a preponderance of age younger than 2 years, boys, and infectious diseases. The mortality mostly occurred from infectious diseases (88.3%) with sepsis, gastroenteritis, and meningitis being the leading causes of death in descending order. The odds of mortality were 4.6-4.7 times higher for children with infectious diseases or for those aged 13-16 years. Hence, policies should be made with general health reforms to improve pediatric health care, as well as to strengthen the already existing preventive and curative programs. The urgent need to strengthen the primary health care system with the enforcement of the national insurance scheme cannot be over-emphasized.
Fig. 1.Diseases that contributed to mortality in the emergency ward (n = 60). The numerical data were as follows: sepsis, 22 (36.7%); gastroenteritis, 10 (16.7%); meningitis, 6 (10.0%); human immunodeficiency virus, 5 (8.3%); malaria, 5 (8.3%); acute respiratory infection, 2 (3.3%); acute renal failure or glomerulonephritis, 2 (3.3%); tuberculosis, 2 (3.3%); undocumented, 2 (3.3%); acute abdomen, 1 (1.7%); poisoning or foreign body, 1 (1.7%); sickle cell disease, 1 (1.7%); and tetanus, 1 (1.7%). 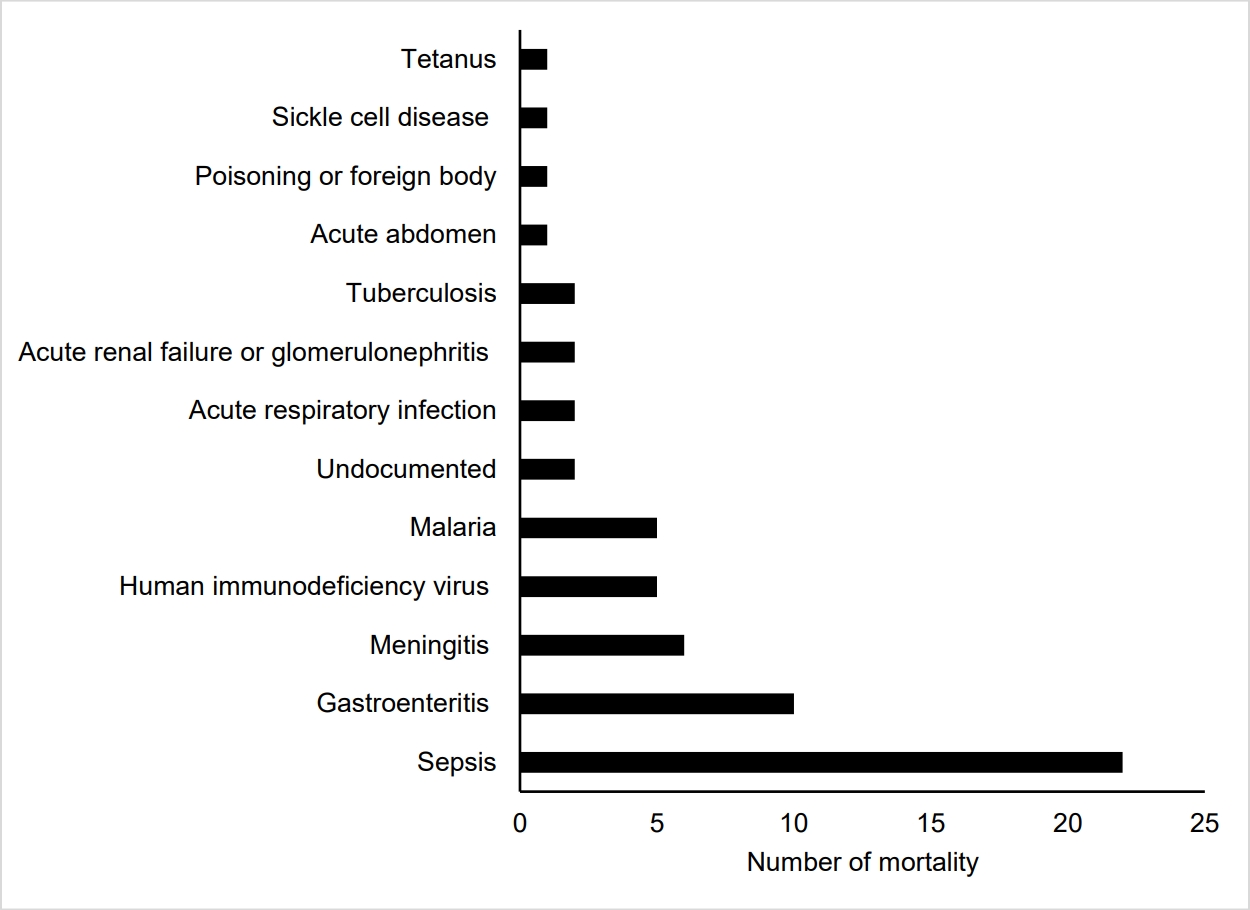
Fig. 2.Case fatality rate of diseases in the emergency ward. The numerical data were as follows: tetanus, 1/1 (100%); human immunodeficiency virus, 5/14 (35.7%); tuberculosis, 2/7 (28.6%); acute renal failure or glomerulonephritis, 2/8 (25.0%); sepsis, 22/111 (19.8%); meningitis, 6/61 (9.8%); undocumented, 2/22 (9.1%); gastroenteritis, 10/115 (8.7%); poisoning or foreign body, 1/12 (8.3%); acute abdomen, 1/18 (5.6%); sickle cell disease, 1/29 (3.4%); malaria, 5/203 (2.5%); and acute respiratory infection, 2/180 (1.1%). 
Table 1.Description of mortality in the emergency ward, Rivers State University Teaching Hospital, Port Harcourt, Nigeria
Table 2.Diagnoses of the children hospitalized to the emergency ward with their age distribution
‡ Diabetic ketoacidosis, osteomyelitis, non-cardiac congenital malformation, peptic ulcer diseases, helminthiasis, dysfunctional uterine bleeding, menorrhagia, laryngomalacia, Hirschsprung’s disease, biliary atresia, upper gastrointestinal tract bleeding, epistaxis, difficulty in hearing, hydrocephalus, hyperemic growth per vagina, acute stroke, stool impaction, scabies, hypoxic-ischemic encephalopathy, hypokalemia, cholelithiasis, lymphoproliferative disorders, uterine prolapse, and urethral stricture following circumcision. References1. World Health Organization (WHO). The global health observatory. Child mortality and causes of death [Internet]. Geneva: WHO: c2022 [cited 2022 Jun 13]. Available from: https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/child-mortality-and-causes-of-death.
2. Whitehead PR. The lived experience of physicians dealing with patient death. BMJ Support Palliat Care 2014;4:271–6.
3. Zhu CP, Wu XH, Liang YT, Ma WC, Ren L. The mortality of patients in a pediatric emergency department at a tertiary medical center in China: an observational study. World J Emerg Med 2015;6:212–6.
4. Lopez E, Udaondo J, Olabarri M, Martinez-Indart L, Benito J, Mintegi S, et al. Mortality in Spanish pediatric emergency departments: a 5-year multicenter survey. Eur J Emerg Med 2017;24:392–7.
5. Tette EMA, Nyarko MY, Nartey ET, Neizer ML, Egbefome A, Akosa F, et al. Under-five mortality pattern and associated risk factors: a case-control study at the Princess Marie Louise Children’s Hospital in Accra, Ghana. BMC Pediatr 2016;16:148.
6. Jofiro G, Jemal K, Beza L, Bacha Heye T. Prevalence and associated factors of pediatric emergency mortality at Tikur Anbessa specialized tertiary hospital: a 5 year retrospective case review study. BMC Pediatr 2018;18:316.
7. Edelu BO, Eze JN, Oguonu T, Ndu IK. Morbidity and mortality pattern in the children emergency unit of the University of Nigeria Teaching Hospital Enugu. Orient J Med 2014;26:73–8.
8. Enyuma CO, Ikpeme OE, Brown-Abang E, Uket H. Morbidity and mortality pattern in a children emergency room in Calabar, Nigeria. J Med Africa 2016;1:6–10.
9. Onyearugha CN, Okoronkwo NC, Onyemachi PE. Mortality pattern in children aged 1-60 months at a tertiary healthcare institution, in Southeast Nigeria. Ann Med Health Sci Res 2020;10:907–11.
10. Ibeziako SN, Ibekwe RC. Pattern and outcome of admissions in the children’s emergency room of the University of Nigeria Teaching Hospital, Enugu. Niger J Paed 2002;29:103–7.
11. Njoku PU, Iloh GU, Dienye PO, Korie FC, Ahaiwe VC. Pattern of paediatric conditions seen in the children emergency room of an urban hospital in South-Eastern Nigeria. GSC Biol Pharm Sci 2020;13:174–80.
12. Singhi S, Jain V, Gupta G. Pediatric emergencies at a tertiary care hospital in India. J Trop Pediatr 2003;49:207–11.
13. Brugnolaro V, Fovino LN, Calgaro S, Putoto G, Muhelo AR, Gregori D, et al. Pediatric emergency care in a low-income country: characteristics and outcomes of presentations to a tertiary-care emergency department in Mozambique. PLoS One 2020;15:e0241209.
14. Duru C, Peterside O, Akinbami F. Pattern and outcome of admissions as seen in the paediatric emergency ward of the Niger Delta University Teaching Hospital, Bayelsa State, Nigeria. Niger J Paed 2013;40:232–7.
15. Okoronkwo NC, ChappJumbo AU. Pattern of morbidity and mortality of childhood illnesses at the children emergency room of Abia State University Teaching Hospital, Aba, Nigeria. East Central Afr Med J 2015;2:70–3.
16. Sa’ad YM, Hayatu A, Al-Mustapha II, Orahachi YM, Hauwa MU. Morbidity and mortality of childhood illnesses at the emergency pediatric unit of a tertiary hospital, north-eastern Nigeria. Sahel Med J 2015;18:1–3.
17. Molyneux EM. Paediatric emergency care in resource-constrained health services is usually neglected: time for change. Ann Trop Paediatr 2010;30:165–76.
18. Ndukwu CI, Onah SK. Pattern and outcome of postneonatal pediatric emergencies in Nnamdi Azikiwe University Teaching Hospital, Nnewi, South East Nigeria. Niger J Clin Pract 2015;18:348–53.
19. Ibeneme CA, Ezuruike EO, Korie FC, Chukwudi NK, Ukpabi IK. Morbidity pattern and outcome among under-fives at the children’s emergency room of Federal Medical Center Umuahia. Niger J Paediatr 2019;46:189–94.
20. Kingwengwe AA, Ndgadi AK, Lukusa PM, Ilunga PM, Ibeki EK, Kyanga PA, et al. Epidemiology of pediatric medical emergencies at the Kindu reference General Hospital (HGRK): state of affairs and perspectives. Open Access Libr J 2019;6:e5715.
21. World Health Organization (WHO). Children: improving survival and well-being 2020 [Internet]. Geneva: WHO: 2020[cited 2022 April 3]. Available from: https://www.who.int/news-room/fact-sheets/detail/children-reducing-mortality.
22. World Health Organization (WHO). Mortality among children aged 5-14 years. Geneva: WHO: 2019[cited 2022 July 11]. Available from: https://www.who.int/news-room/fact-sheets/detail/mortality-among-children-aged-5-14-years.
AppendicesAppendix 1Univariable analysis
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

 |
 |