Introduction
As a rare complication of maxillofacial and dental surgery, subcutaneous emphysema occurs as a result of an influx of air into soft tissue through a surgical defect. Mediastinal emphysema during dental care was first reported in 1900 [1]. Reports of subcutaneous emphysema caused by tooth extraction have been reported on rare occasions, but the incidence of iatrogenic subcutaneous emphysema has risen since the introduction of high-speed drilling equipment in the 1960s. Severe emphysema may spread to the face, neck, mediastinum, and thorax, causing cervical emphysema, pneumomediastinum, and pneumothorax [2]. We report a case of subcutaneous emphysema with facial edema during restorative dental treatment.
Case
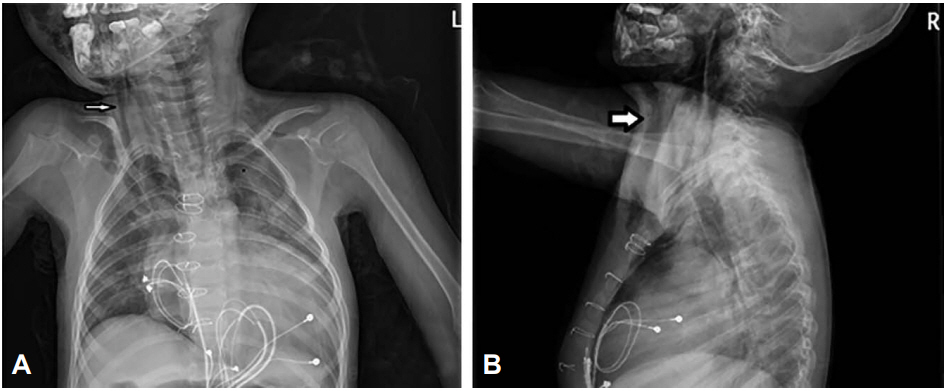
A 5-year-old girl was transferred to our hospital after developing rapidly progressive facial edema while receiving dental treatment under oral sedation with midazolam rather than N2O gas anesthesia. She had an implanted pacemaker for dilated cardiomyopathy, and had developed ischemic hypoxic encephalopathy due to cardiac arrest at 12 months of age. The patient was undergoing resin restoration of the left mandibular first and second primary molars, pulpectomy of 3 upper anterior teeth, root canal surgery, and composite resin restoration of both canines for 2 hours. The dentist continued treatment despite the development of facial edema, thinking that the condition was transient. However, the edema progressed and the patient was transferred to our hospital. Although she could not verbalize her pain, she was agitated and dyspneic. The initial vital signs were as follows: blood pressure, 90/70 mmHg; heart rate, 114 beats per minute; respiratory rate, 32 beats per minute; temperature, 37.3°C; oxygen saturation, 98% at 1 L/min of oxygen via nasal cannula. We observed swelling of both eyelids and crepitus with swelling from the right cheek to the neck, both clavicle, and upper chest upon palpation, but there was no Hamman’s sign. Plain cervical radiographs showed a linear layer of air in the retropharyngeal space, and plain chest radiographs also showed subcutaneous emphysema with pneumomediastinum in the upper chest (Fig. 1). Head computed tomography showed a band of air in both periorbital areas and subcutaneous tissue of both cheeks (Fig. 2). After hospitalization, the patient was administered oxygen via nasal cannula and ]intravenous ampicillin/sulbactam (60 mg/kg/day). On day 3, the extensive edema began to subside, and plain cervical radiograph confirmed that the linear air column in the retropharyngeal space was much reduced. On day 6, all visible swelling subsided, and the patient was discharged. Complete recovery without complications was confirmed during outpatient follow-up 7 days after discharge (Fig. 3).
Discussion
Subcutaneous emphysema may rarely occur during dental care. Most cases of subcutaneous emphysema result from high pressure air created by a high-speed dental drill and air-and-water dental syringe. Air or water generated by these devices may enter the subcutaneous layer through a surgical wound [3]. Air, water, bacteria, and foreign bodies may contaminate these spaces.
Heyman and Babayof [4] reported 75 cases of subcutaneous emphysema and pneumomediastinum that occurred after dental treatment between 1960 and 1993, and Arai et al. [5] reported 47 cases published between 1994 and 2008. According to these articles, the most frequent cause was tooth extraction (51 of 122 cases, 41.8%), followed by restorative dentistry (40 of 122 cases, 32.8%), root canal treatment using H2O2 (14 of 122 cases, 11.5%), and periodontal treatment (11 of 122 cases, 9.0%).
Tooth extraction may expose deep structures by causing extensive damage of soft tissue and bone, which may facilitate air infiltration. Moreover, long treatment duration may cause air accumulation, increasing the risk of subcutaneous emphysema. Although the patient in the present case was only undergoing minor procedures, as opposed to invasive treatment such as tooth extraction or bone removal, she developed facial edema as well as pneumomediastinum. There were 2 potential causes of her subcutaneous emphysema. First, the restorative treatment was not as extensive as extraction, but did weaken gingival attachments, possibly enabling air influx through the gingival sulcus. Second, compressed air used for drying during root canal irrigation may have entered the periapical tissue and caused the emphysema. Moreover, subcutaneous emphysema can develop if H2O2 injection is inaccurate or when the gas is directly injected into soft tissue through a pathway in the buccal bone created by a previous infection of the periapical area [6].
Eleven of the 122 cases reported by the above 2 studies involved children, accounting for 9% of all cases. In general, the quality and amount of soft tissue and bone are high in children, and the duration of dental treatment is shorter, lowering the risk of subcutaneous emphysema [7]. However, treatment can be delayed in children with difficulty communicating, necessitating more careful observation.
Facial swelling during dental treatment can be caused by an allergic reaction, hematoma, cellulitis, or emphysema, and the dentist in the present case continued treatment despite facial swelling, assuming that it would be transient. However, the dentist stopped treatment and transferred the patient to our hospital when the swelling rapidly worsened, affecting the scalp and upper chest. Epinephrine was injected in another case in which subcutaneous emphysema was mistakenly treated as an allergic reaction [8]. When a large amount of air enters the deep neck space, it may cause severe cardiac and respiratory problems. Moreover, air infiltration of the retropharyngeal space may cause airway compromise [9]. Thus, providing appropriate treatment based on an accurate diagnosis is essential. Subcutaneous emphysema quickly spreads to the scalp, neck, and chest, and is easily distinguished from other conditions due to characteristic crepitus on palpation.
Most facial subcutaneous emphysema subside spontaneously in about 1 week [10]. However, subcutaneous emphysema affecting the neck, mediastinum, and thorax can be life-threatening. Upper airway obstruction can also develop with severe air trapping in the retropharyngeal and prevertebral space, and pneumomediastinum can affect cardiopulmonary function due to the air compression. Hence, patients with subcutaneous emphysema must be hospitalized for 24-hour monitoring of vital signs and overall status, and prophylactic antibiotics should be considered to prevent local or systemic infections, especially acute mediastinitis. Oxygen therapy should also be considered, as it may facilitate absorption of trapped nitrogen by lowering the surrounding partial nitrogen pressure [2].
Subcutaneous emphysema in the present case is believed to have occurred as a result of high-pressure air generated by a high-speed hand piece and root canal irrigation using H2O2. The entity is painful, and would have been diagnosed sooner if the patient was conscious or able to verbalize. Diagnosis was delayed for 2 hours because the patient had difficulty communicating, and assessment was made at a more advanced stage. Although it is unknown whether subcutaneous emphysema is more likely to occur in patients with poor communication, it can get worse in them. To our best knowledge, this is the first case report of subcutaneous emphysema during dental treatment in Korean children. Dentists should monitor pediatric patients more carefully, especially those who are unable to communicate well, even during minor procedures. In addition, pediatricians should be aware of the possibility of subcutaneous emphysema during dental treatment, to enable prompt diagnosis and appropriate treatment.